Biological engineers from Massachusetts Institute of Technology (MIT) have developed a multi-tissue model that allows them to analyze the associations between the immune system and different organs, on a dedicated microfluidic platform embedded with human cells.
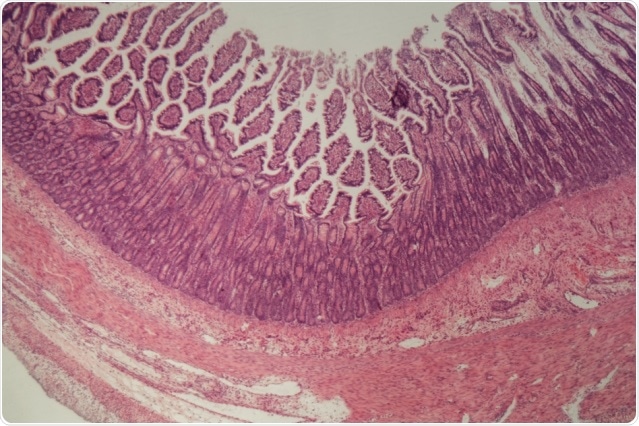
MIT engineers have devised a new approach to studying complex diseases such as ulcerative colitis, which causes inflammation of the intestines. Image Credit: MIT.
With the help of this multi-tissue model, also known as “physiome on-a-chip or “organs-on-a-chip,” the researchers were able to examine the role played by the circulating immune cells in various inflammatory diseases, including ulcerative colitis.
The researchers also observed that a metabolic byproduct produced by bacteria dwelling in the human gut have a crucial role to play under these inflammatory diseases.
We’ve shown that now you can start to attack some of these really thorny, chronic inflammatory diseases by designing experiments in these organs on chips.”
Linda Griffith, Study Senior Author and Professor, Departments of Biological Engineering and Mechanical Engineering, MIT
Griffith is also the School of Engineering Professor of Teaching Innovation.
Described recently in the Cell Systems journal, this technique could also make it possible to analyze several other complex diseases, stated the team.
Now we have options to really decrease or increase the level of disease complexity, under controlled and systematic conditions.”
Martin Trapecar, Study Lead Author and Postdoc, MIT
Complex models
Almost two decades ago, Griffith’s laboratory originally began to work on the human liver model called the “liver chip.” This model, comprising engineered human liver tissue cultured on a dedicated scaffold, can be utilized for testing the toxicity of drugs.
Of late, Griffith has been working on small-scale models of several interconnected organs, referred to as microphysiological systems (MPS). Back in 2018, she reported the creation of a platform through which interactions between a total of 10 organs could be modeled at a time.
Such devices are suitable for studying complicated diseases, including those that are affected by the immune system, involve multiple organs, or cannot be implicated by an insignificant number of genes or a single gene.
We wanted to build technologies that would let you connect several organ systems together, so that we could start to develop new tools to combat chronic inflammatory diseases. In drug development, the field really struggles with anything that’s not a single-gene disease.”
Linda Griffith, Study Senior Author and Professor, Departments of Biological Engineering and Mechanical Engineering, MIT
In the latest Cell Systems research, Griffith and Trapecar went on to model the interactions that occur between a pair of organs, for example, the liver and the colon. The researchers also wanted to investigate how the immune system, specifically T cells, has an impact on those organs.
It is well known that up to 80% of patients suffering from a chronic liver autoimmune disease, known as primary sclerosing cholangitis, also have inflammatory bowel disease (IBD). Also, patients suffering from IBD are at more risk of developing autoimmune disorders of the liver.
The novel system consists of colon cells that were extracted from patients suffering from ulcerative colitis, together with healthy liver cells.
Upon connecting these tissues, the scientists discovered that the physiological behavior of these tissues changes entirely when compared to the ones that were isolated.
Upon exposing the tissue to healthy liver cells, inflammation in ulcerative colitis gut tissue reduced. Cellular pathways and genes responsible for immune function and metabolism turned out to be more active in both organs at the same time.
The scientists subsequently introduced two types of T cells to the new system—TH17 cells, which trigger inflammation, and CD4+ T regulatory cells, which suppress other immune cells. When these T cells were added to the liver-gut interaction, inflammation increased rapidly and certain traits of both autoimmune liver and IBD diseases were reproduced.
The scientists finally decided to examine the promising role of molecules known as short-chain fatty acids (SCFAs) in inflammatory diseases.
Molecules like these are created by pathogens in the human gut as they feed on fiber that was not digested. SCFAs, which contain acetate, propionate, and butyrate, are generated in large amounts and are responsible for around 10% of humans’ day-to-day energy requirements.
Although such compounds have several beneficial impacts in the human body, such as decreasing inflammation, some studies performed in the recent past have indicated that the same SCFAs can also be harmful by activating inflammation.
The latest study carried out by MIT discovered that when SCFAs are added to the model of ulcerative colitis, they considerably aggravated inflammation all through the gut and liver, but this happens only when T cells already exist.
“The hypothesis we formed, based on these studies, is that the role of short-chain fatty acids seems to depend on how much the adaptive immune system (which includes T cells) is involved,” added Trapecar.
That means, during the initial stages of inflammation, SCFAs can help decrease inflammation, specifically when T cells are not largely involved.
However, when several effector T cells are recruited, SCFAs activate them to be much more inflammatory. While this could prove handy during infection cases to aid the body to avert invaders, it can also speed up autoimmune diseases.
Modeling brain disorders
The research emerged from a similar study where the scientists intended to examine the interactions that occur between the brain, liver, and gut.
A new study conducted by Sarkis Mazmanian, a professor of microbiology at Caltech, demonstrated that in a mouse model of Parkinson’s disease, germ-free mice later developed signs of this disease when compared to those kept under normal conditions.
The research indicated that SCFAs created by bacteria might potentially contribute to the observed phenomena and development of the disorder.
At present, Griffith’s laboratory is working to utilize the MPS system to gain a better understanding of the association between Parkinson’s disease and SCFAs. The scientists have also planned to analyze other complicated medical conditions and hope that their study outcomes will help direct the development of novel therapies for difficult-to-treat disorders.
“You need very complex models,” added Griffith. “You can certainly get hypotheses from animal models, but to go forward in drug development, you need better ways to identify targets that build on samples from human patients.”