The main function of non-circulating memory T cells is to offer local protection against re-infection. These cells play a key role in chronic transplant rejection, according to researchers from the University of Pittsburgh School of Medicine in an article recently published in the Science Immunology journal.
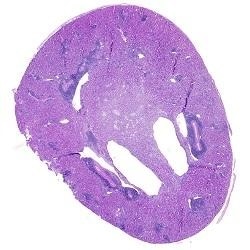
Transplanted kidney stained with a blue dye shows signs of inflammation. Image Credit: Martin Oberbarnscheidt.
The researchers demonstrated that these “tissue-resident memory T cells” are detrimental in situations where antigens recognized by the cells are present in the body for an extended period, including the cases of a tissue or organ transplant. This discovery is a major step forward in the development of more improved treatments to help avoid organ rejection in transplant recipients.
Tissue-resident memory T cells serve an important surveillance function. If these cells encounter the same pathogen more than once, they can help quickly eliminate it. But studying these cells in transplants gives us a unique opportunity to look into what happens when the antigen persists--a new organ transplant is a big piece of tissue which, unlike an infection, stays in the body for a long time.”
Martin Oberbarnscheidt, MD, PhD, Study Co-Senior Author and Assistant Professor of Surgery, University of Pittsburgh
T cells, a subset of immune cells crucial in the development of acquired immunity, have long been recognized by transplant surgeons and immunologists to play a key role in the acute rejection of a transplanted organ. However, the role of resident memory T cells in transplant rejection was previously overlooked, until now.
Resident memory T cells turn from being protective against an infection into a problem in a transplant setting as they fight off a life-saving organ. It's an elephant in the room--T cells are present at a chronic stage of the kidney transplant rejection, but no one knew if these cells were functional.”
Khodor Abou-Daya, MD, Study Lead Author and Research Assistant Professor, Department of Surgery, University of Pittsburgh
The researchers used a mouse model of kidney transplantation and demonstrated that activated T cells that penetrate a transplanted organ generally morph into resident memory T cells over time.
They found that if the blood circulation of two mice, which received identical kidney transplants, are surgically conjoined, the memory T cells that form in transplanted organs do not migrate from one mouse to the other.
In a similar way, if a transplanted kidney is subsequently taken out and re-transplanted into another mouse, the resident memory T cells remained in the transplanted kidney and did not spread anywhere else in the recipient’s body, indicating that these cells remain permanently in the tissue.
It is also worth noting that in spite of the presence of the ubiquitous antigen, the tissue-resident memory T cells did not become “exhausted,” as is usually the case in these T cells at the time of chronic infections or in tumors.
Rather, the cells continued to remain functional, spreading and generating signals that maintained the immune response for an extended period. Furthermore, the formation of these cells precipitated the rejection of a kidney graft.
There is an assumption that T cells in transplanted organs or tissues are exhausted and dysfunctional and may not contribute significantly to tissue rejection. Our work shows that tissue-resident memory T cells are functional and destructive.”
Khodor Abou-Daya, MD, Study Lead Author and Research Assistant Professor, Department of Surgery, University of Pittsburgh
Particularly targeting these cells could enhance the outcomes of clinical transplants while maintaining the ability of the immune system to combat infections, thereby decreasing the side effects of existing systemic immunosuppressive treatments.