The Hubrecht Institute's Organoid group created the first organoid model of the human conjunctiva. The function of these organoids is mimicked by the human conjunctiva, a tissue involved in the formation of tears. Using their new model, the researchers identified tuft cells as a novel cell type in this tissue.
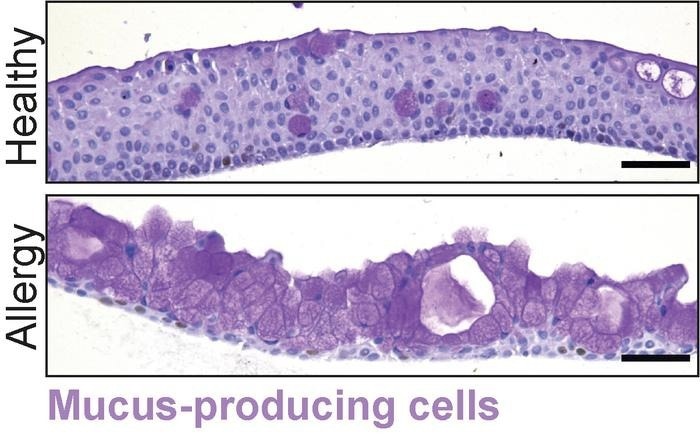 Under allergy-like conditions, the number of mucus-producing cells increases. Image Credit: Marie Bannier-Hélaouët
Under allergy-like conditions, the number of mucus-producing cells increases. Image Credit: Marie Bannier-Hélaouët
Tuft cells may contribute to allergies because they grow more prevalent in environments that resemble allergies. Nowadays, medications for a number of conjunctival illnesses can be tested using the organoid model. The results are reported in Cell Stem Cell.
Tears are produced in the eyes to shield them from wounds and diseases. These tears are partially produced by the conjunctiva, a tissue that covers the inside of the eyelids and the white of the eye. It contributes to the formation of tears by releasing mucus. This mucus shields the ocular surface from infections and enables tears to adhere to it.
Limited Treatment Options
A number of illnesses and conditions, including infections, allergies, cancer, and dry eye syndrome, impact Conjunctiva. When this tissue malfunctions severely, blindness may result. Research on the human conjunctiva's role in health and illness has been limited because there has not been a reliable model of the organ until now. Thus, the therapy choices for conditions affecting the conjunctiva are restricted.
First Model
The Organoid group set out to create the first human model of this sort of tissue to obtain a further understanding of the structure and function of the conjunctiva. They cultivated human conjunctival cells into three-dimensional structures in a dish. These microscopic formations resemble actual human conjunctiva and are known as organoids.
Once we had these functioning organoids, we wanted to know how the conjunctiva is involved in the production of tears. Also, we discovered that the conjunctiva makes antimicrobial components and therefore contributes to tear production in more ways than simply making mucus.”
Marie Bannier-Hélaouët, Lead Researcher, Hubrecht Institute
Allergies
Then, to simulate allergies, the researchers changed the environment of the plate containing the tiny conjunctivae.
The organoids started to produce completely different tears: there was more mucus, but there were also more antimicrobial components; under these conditions, they also found a new cell type in the organoids: tuft cells are similar cells that have been discovered in other tissues, but not in the human conjunctiva.”
Marie Bannier-Hélaouët, Lead Researcher, Hubrecht Institute
In the allergy-like environment, the number of tuft cells increased, indicating a potential involvement for these cells in the ocular response to allergens. The recently created organoid model makes it possible to study conditions that impact the conjunctiva.
Marie Bannier-Hélaouët said, “We can use our model to test drugs for allergies or dry eye disease, for example.”
In the long term, it might even be feasible to create new conjunctivae for patients suffering from genetic diseases, ocular burns, or ocular malignancies.
Marie Bannier-Hélaouët concluded, “We are now running preclinical studies in rabbits to assess whether this approach is feasible and helpful.”
Sources:
Journal reference:
Marie Bannier-Hélaouët., et al., (2024). Human conjunctiva organoids to study ocular surface homeostasis and disease. Cell Stem Cell. doi.org/10.1016/j.stem.2023.12.008