Biodegradable polymeric scaffolds are of high interest for regenerative medicine applications. If tissues become damaged, such scaffolds can be 3D-printed to provide temporary stabilization, and since they degrade over time there is no need to extract the scaffold at a later stage.
The degradation is most efficient if cells from surrounding tissues grow into the polymer scaffolds. With the aim to understand which features of polymeric scaffolds attract cells, a research collaboration from Italy and Slovakia studied the adhesion of epithelial cells to surface-coatings of different biodegradable, 3D printable polymers.
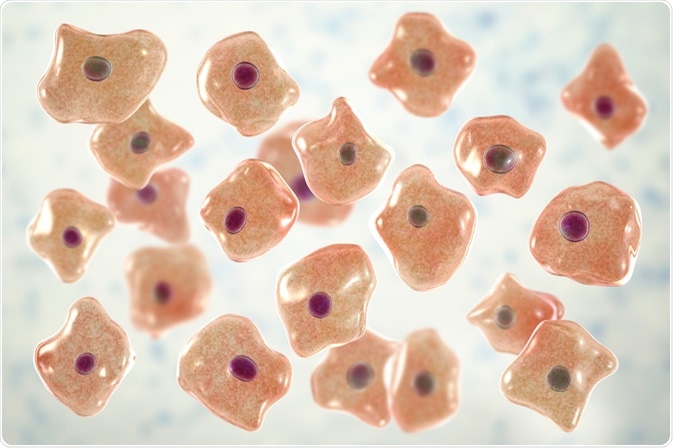 Image Credit: Kateryna Kon/Shutterstock.com
Image Credit: Kateryna Kon/Shutterstock.com
Open wounds heal slowly if they are not stitched or glued to close the void they leave. After healing, scars are a common remnant from the injury. Similar injuries can also occur in the urethral tract that carries urine from the bladder to the outside of the body.
Common causes are trauma events, where forceful impacts cause ruptures in the urethra. The subsequent swelling and scarring can constrain the urethral tract and consequently, urine cannot leave the body easily. Even worse, if the urethral walls are damaged urine can reach the surrounding tissue and cause inflammation.
A common treatment of urethral traumas is to insert catheter tubes through the urethra and into the bladder, to hold the tract open, and provide an exit for urine.
While this gives the surrounding tissue time to heal, it can be necessary to leave the catheter inside the urethral tract for several months, and the catheter can cause irritations in the bladder. Once the catheter is removed, scarring tissue might again constrain the urethral tract and needs to be removed surgically.
Research on regenerative medical treatments has suggested that 3D-printed, biodegradable polymer scaffolds could provide a great benefit. These could be printed into shapes that keep the urethral tract temporarily open, while they would disappear with time by biodegradation.
For the degradation to be efficient, cells should adhere to the artificial urethral tract, grow into the scaffold, and successively replace the polymeric material with native extracellular substances such as collagen.
Scientists from Italy and Slovakia, led by Professors Federica Chiellini (Pisa) and Vladimir Frecer (Bratislava), investigated the adherence of cultured human bladder epithelial cells (HBLAK) to different biodegradable, 3D-printable polymer films.
They found that computational molecular mechanics models of the transmembrane protein integrin binding to polymer surfaces predicted well the polymers to which HBLAK cells adhered strongest in experiments, while no correlation was observed across all tested polymers.
Testing polymers for optimal cell adherence
The investigators studied five polymers, namely the polysaccharides hyaluronic acid (HA) and amylose, the extracellular matrix protein collagen, and the organic acid-based polymers poly(hydroxybutyric acid) (PHB) and poly(lactic acid) (PLA).
Polymer layers were prepared by solvent casting, in which the polymers were dissolved in a solvent (i.e. water or chloroform), the solutions transferred onto a glass slide, and polymer films remained after drying of the solvent. For adherence assays, HBLAK cells were seeded onto these polymer films, the excess cell culture liquid was washed off after 30 minutes and bound cells were quantified by metabolic activity assays.
The experimental adherence data was compared to a computational force field model. In this model, the scientists constructed planar sheets of the polymers. The sheets were characterized by different surface charges and hydrophobicities, depending on which polymer was tested.
To represent cells in the models, the scientists programmed a domain of integrin, a transmembrane protein of HBLAK cells. Integrin’s native function is the binding of extracellular collagen matrices, and the computer models predicted from electrostatic interactions how the protein can interact with and bind to the polymer surfaces. As a result, binding energies between integrin and the polymers were calculated to predict the strength of the interaction.
Polar residues drive cell adhesion
The scientist demonstrated experimentally that the HBLAK cells adhered strongest to the PHB and amylose films. This correlated with their prediction from the computer models and the researchers concluded that polar groups on the polymer sheet surface were facilitating the binding of integrin.
However, the model could not predict the experimental trend of HBLAK adherence to all of the five polymers. Since modeling planar polymer films and a single integrin domain is a strong simplification, more complex computer models could refine the predictive power of the force field model.
Having identified experimentally that PHB and amylose support strong cell adherence, the researchers suggest that these polymers could be used in artificial tissue scaffolds to attract endothelial cells.
Since however such scaffolds need to simultaneously provide stability, they suggest PHB or amylose as a component in composite materials containing also stiffer polymers, such as collagen fibers although these did not support good cell adhesion themselves in their study.