There are 206 bones in an adult human. In addition to multiple types of fractures, several medical conditions require bone healing and growth. These conditions include age-related degeneration, cancer, and bone deformities.
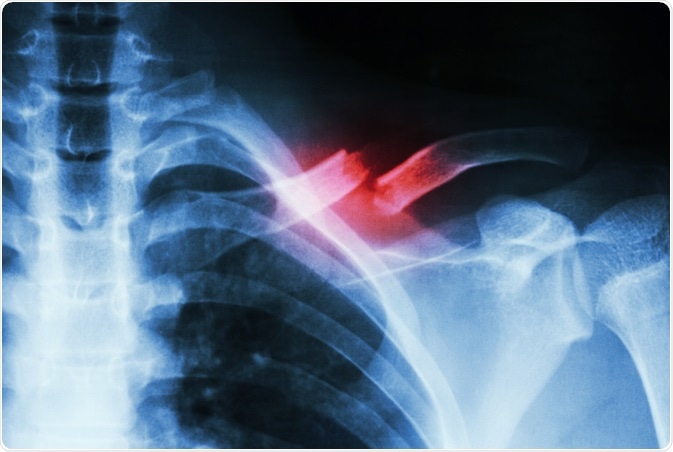
Image Credit: Puwadol Jaturawutthichai/Shutterstock.com
Most of these require invasive surgery and long healing times with a relatively high risk of infection. Techniques which can reduce healing time and minimize invasive surgery will be beneficial, which means that research into biomaterials that support these goals is essential.
Bone defects are a significant cause of disability. Longer human lifespans and bone pathology have highlighted the need for biocompatible materials with good mechanical properties. Regenerative medicine incorporates both biological sciences and fundamental engineering. Biomaterials that have good mechanical properties and also promote the growth of new bone cells are the aim. These will require bone engineering and tissue engineering to be successful.
The history of “artificial bone support” goes back a long way. As early as the 16th century, Aztec medics were using wooden implants to aid bone repairs. In the 18th century, surgeons used ivory as bone support to stabilize fractures and encourage regeneration. Metal implants were used in the first world war to treat war wounds. Initially, stainless steel was used for implants such as screws, etc. Titanium is now preferred because stainless steel corrosion products can be toxic.
The prime function of metallic inserts and supports is as a scaffold to support bones which can then be allowed to grow back naturally. Titanium can sometimes be made to be bone-friendly, but it is inert and does not actively promote bone regeneration. Metal inserts can give strong support but promote weak growth. Metal inserts can also cause pain, skin itchiness, and feel cold when the weather is cold. Biomaterials offer the possibility of a combination of support and growth promoters to be included in a single product. The goal of biomaterials is to stimulate faster healing or regrowth while simultaneously giving support to the bone in question.
Bone is a complex 3d structure that includes inorganic as well as organic materials. There are two main types of bone cell structure: cortical bone, which is the mechanical strength, and trabecular bone, which is where bone growth and regeneration occurs. The mechanical strength of bones is provided mainly by Calcium Hydroxyapatite (Ca10(PO4)6, a common steam boiler scale), but other minerals can be present in bone in small amounts. Bone also includes several different types of specialist cells.
Some of the most interesting cells in the bone are mesenchymal cells. These are stem cells found in the bone marrow. Incorporating mesenchymal cells into biomaterials allows the product can act as a scaffold for bone growth and promote the formation of new bone cells from any of the different kinds of bone cells.
An ideal biomaterial will mimic bone structure and composition. It will be biocompatible with the host and have no immunology triggers. It will also be biodegradable and be able to be reabsorbed after the new bone is formed. The bone structure it creates will promote bone cell growth but also differentiation in the new cells formed.
There are three main tissue engineering strategies, and the choice of method will depend on the severity of the bone condition which is to be treated.
- Direct biomaterial implant
- Using freshly harvested stem cells (grown in a lab or concentrated from a live sample)seeded on a biomaterial
- Cell harvesting and growth in a lab and seeded into a biomaterial with growth agents.
Biomaterials can be derived naturally or created artificially. Artificially synthesized materials have the advantage of being able to be made to order, and they can be created without any immunology triggers making them safer to implant. Artificial biomaterials tend to be one of three types;- Ceramic materials, Polymer biomaterials, Composite biomaterials are often a composite of the other two types.
Ceramic biomaterials
Ceramics are usually biocompatible, corrosion, and compression resistant; however, they are often also brittle. Ceramics often use tricalcium phosphate as a base; small amounts of Strontium or Magnesium can add strength. Hydroxyapatite can also be used in biomaterials. Some studies have used magnetically activated ceramics that can be triggered to form support when in place.
Polymer biomaterials
Polymers can be natural or synthetic. Natural polymers such as collagen are used to mimic natural bone structures. Collagen is the most common protein in vertebrates, and it is very common in bone tissue. It is often used in conjunction with ceramics such as bone cement (Calcium Phosphate) to enhance the healing effects.
Another natural polymer-based treatment for bone regeneration is demineralized bone. Demineralized bone is harvested from living organisms, possibly the patient, and is rich in collagen and growth factors. If the patient’s bone is used, there will be no immunology issues. If it is from another person or organism, then there could be biocompatibility issues. Harvesting biomaterials from an already traumatized patient can have a significant impact on the process.
Synthetic polymers for bone regeneration are attractive as they can be manufactured independently of the traumatized patient. The challenge is to devise a biomaterial that has suitable mechanical properties and encourages bone growth with no immune reactions. Good osteoconductivity and mechanical strength have been achieved using a copolymer of polyglycolide and polylactic acid.
An additional challenge with synthetic polymer products is to ensure that they are biodegradable and that when they degrade, they should not create local pH changes. Synthetic polymer biomaterials have been used in some situations to deliver drugs to bone tumors.
Composite biomaterials
A biomaterial that combines ceramic and polymer materials can have good load-bearing and mechanical properties and be good for tissue engineering. Tissue engineering uses a combination of stem cells, biomaterial scaffolds, and growth agents to speed up bone regeneration. Things like porous hydroxyapatite and collagen mixes can be successful especially if used with mesenchymal cells. Many biomaterials are designed to mimic natural bone’s ability to heal by copying bone biology.
All new biomaterials need clinical trials before they can be widely used, which slows development and implementation. There are numerous projects around the World working on new biomaterials for bone healing.
A French team has developed a product based on silanized hydroxypropylmethylcellulose composite with calcium phosphate. This has good mechanical properties and is injectable. An advantage of this method is that no large incisions are required to deliver the product to the trauma area.
Duke University in the USA has developed a technique of 3d printing metal and polymer scaffolds for bone trauma.
Kings College in London has developed a process where stem cells are removed and grown in a lab and then implanted on a fracture in a biomaterial bandage to speed healing.
Many other researchers are working on synthetic biocompatible polymers which are easily manufactured and deployed. In addition to developing new substances, researchers are also developing innovative ways of developing the biomaterials to the bone trauma site
Sources:
- Bone regeneration: current concepts and future directions Rozalia Dimitriou, Elena Jones, Dennis McGonagle & Peter V Giannoudis
https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-66
- Innovative Biomaterials for Bone Regrowth Maria Rosa Iaquinta, Elisa Mazzoni, Marco Manfrini, Antonio D’Agostino, Lorenzo Trevisiol, Riccardo Nocini, Leonardo Trombelli, Giovanni Barbanti-Brodano, Fernanda Martini, and Mauro Tognon https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6387157/
- Recent Trends in the Development of Bone Regenerative Biomaterials Guoke Tang, Zhiqin Liu, Yi Liu, Jiangming Yu, Xing Wang, Zhihong Tan, and Xiaojian Ye https://www.frontiersin.org/articles/10.3389/fcell.2021.665813/full
- A simple and effective approach to prepare injectable macroporous calcium phosphate cement for bone repair: Syringe-foaming using a viscous hydrophilic polymeric solution WeizhenLiu,, SophieSourice, PaulPilet, GildasRethore, KhalidKhairoun, Jean- MichelBouler, FranckTancret, www.sciencedirect.com/science/article/abs/pii/S1742706115302312
Further Reading