The human gut microbiome consists of the microbes residing in the digestive tract of humans and makes up a significant proportion of the total human microbiome.
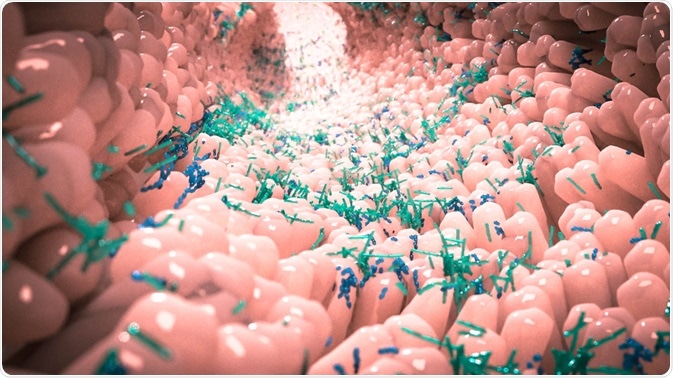
Image Credit: Alpha Tauri 3D Graphics/Shutterstock.com
The relationship between gut flora and the body is mutualistic, benefiting both the host and microbes — examples include the fermentation of dietary fibers and the synthesis of vitamins B and K.
Recent research has indicated the role of gut microbes in the regulation of helper T cells and regulatory T cells. Therefore, specific microbial species can have a role in the suppression or promotion of the immune response against the presence of a specific antigen.
Many studies have linked allergic reactions to differences in microbiome composition, with certain microbes providing protective properties against certain allergies.
Hygiene hypothesis
The role of microbes in providing a protective effect against infectious agents and immunological disorders was first proposed in 1978 by Strachan. An inverse correlation was observed between hay fever and the number of older siblings in British children.
Many further epidemiological studies in high-income countries have correlated reductions in infectious diseases with increases in allergies and immunological disorders.
Increased levels of hygiene have directly contributed to reductions in infectious diseases, however, as a side effect, there is reduced contact to a diversity of microbial species in childhood. This results in the microbial composition of individuals in high-income countries being significantly less diverse than for those in low- and middle-income countries.
The hygiene hypothesis states that, while increasing hygiene protects against morbidity and mortality from infectious agents, the reduced diversity of the microbiome confers an increased risk of developing allergies and immune disorders.
Role of the gut microbiome in food allergies
Recent studies have taken advantage of 16S rRNA sequencing to determine differences in the gut microbiome. This allows comparisons between the gut microbiome composition of allergic and non-allergic children.
A study from the Consortium for Food Allergy Research of 141 children with egg allergy, found significant differences in microbiome composition compared to healthy controls. Genera from Lachnospiraceae, Streptococcaceae, and Leuconostocaceae families were particularly abundant.

Image Credit: Photoroyalty/Shutterstock.com
Furthermore, differing gut microbiome composition has been associated with the clinical development of food allergy. A study in Japan sequenced the microbiota of 56 infants at age 2 months.
The 14 children who reported wheat, milk, soy or egg allergies by the age of 2 years, had significantly fewer microbes of the genera Leuconostoc, Weissella and Veillonella compared to healthy participants.
There appear to be specific implications of the gut microbiome composition in early infancy and the development of food allergies. A Canadian study showed the increased richness of the gut microbiome at age 3 months was associated with reduced risk of developing food allergies by 12 months, whereas the composition of the gut microbiome at 12 months had no association with food allergies.
The potential use of probiotics to prevent food allergy
The gut microbiome is developed through the acquisition of microbes in early childhood. This is influenced by both genetic (host physiology) and environmental factors. Diet is increasingly thought of as a key environmental element in this process, particularly the use or non-use of breastfeeding.
Certain dietary intervention studies have shown that supplementing a child’s diet with probiotics in their first two years is associated with a significantly lower prevalence of allergy.
Probiotics contain non-digestible compounds that affect the composition/activity of the gut microbiome, promoting a positive effect on the host.
Systematic reviews in this area have shown that, while positive results have been observed, more evidence is required before this approach becomes a routine prevention strategy. Additional statements from the World Health Organisation (WHO) mention the ‘very low quality of evidence’ to date.
This is partly because many different factors affect the allergic response and the microbiome has many other roles in the healthy body. The mechanisms by which specific gut microbes protect against different food allergies are also largely unknown.
Other solutions
Intentionally contaminating a healthy child with an infective agent, to prevent any potential allergic responses, is out of the question. However, the use of bacterial, parasitic or viral extracts may provide a less risky model to promote a strong immune system.
This would require a greater characterization of the mechanism of the development of an allergic response. Additionally, any other interactions between the extract and the host or microbiome would need to be determined to ensure the safety of any such prophylaxis.
The relation between the gut microbiome and the human body is a highly complex ecosystem that has been relatively understudied. This is a current area of interest for microbiologists keen to understand how specific interactions between the body and microbiome provide beneficial effects.
Further evidence in this area may lead to novel techniques to prevent the development of food allergy in early childhood.
References
- Bunyavanich, S. and Berin, M. C. (2019) ‘Food allergy and the microbiome: Current understandings and future directions’, Journal of Allergy and Clinical Immunology. Mosby Inc., pp. 1468–1477. doi: 10.1016/j.jaci.2019.10.019.
- Miqdady, M. et al. (2020) ‘Prebiotics in the infant microbiome: The past, present, and future’, Pediatric Gastroenterology, Hepatology and Nutrition. Korean Society of Pediartic Gastroenterology, Hepatology and Nutrition, 23(1), pp. 1–14. doi: 10.5223/pghn.2020.23.1.1.
- Okada, H. et al. (2010) ‘The “hygiene hypothesis” for autoimmune and allergic diseases: An update’, Clinical and Experimental Immunology, pp. 1–9. doi: 10.1111/j.1365-2249.2010.04139.x.
- Riiser, A. (2015) ‘The human microbiome, asthma, and allergy’, Allergy, Asthma and Clinical Immunology. BioMed Central Ltd. doi: 10.1186/s13223-015-0102-0.
Further Reading