In this article, the influence of the gut microbiome and its composition on obesity is discussed.
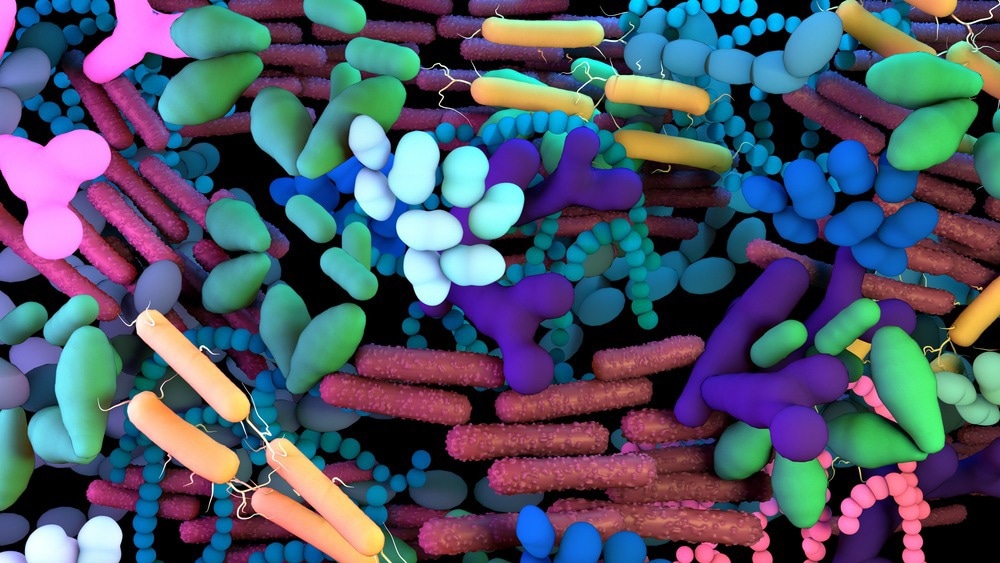
Image Credit: Design_Cells/Shutterstock.com
Microbiome Vs. Microbiota
Research into the human microbiome and microbiota continues to evolve, but a lack of consensus on the definitions of these terms remains. Based on the contributions of experts, the microbiota is defined as the environment comprising organisms such as bacteria, archaea, fungi, algae, and protists. In contrast, the microbiome includes the ‘theatre of activity’, i.e., the genetic and structural features such as nucleic acids, lipids, and polysaccharides. Another term used is the metagenome which are the genomes/genes of the microorganisms of the microbiota.
What is the Gut Microbiome
The gut microbiota is the largest microbial community, part of the human microbiota, found in the gastrointestinal tract. The microbes that inhabit the gut share a symbiotic relationship with the host, which is regulated by a multitude of interactions that involve producing energy and vitamins such as vitamin K and folate.
They also have roles in neuro-immune-inflammatory signaling and immunity. For instance, there is a mucus and epithelial layer that forms the gut barrier between the host and the environment. If disrupted, it increases permeability to microbes which may have virulence factors that can contribute to inflammatory responses.
There is a plethora of research that describes an intricate connection between the intestinal microbiome and health. Factors such as antibiotic consumption, nutrition, stress etc., can cause ‘dysbiosis’ in the gut microbiome, which means that the microbiota stops functioning correctly to maintain health and, more importantly, differentiate between harmful and helpful microbiota. This can become very harmful to the host and cause several health problems, such as Clostridium difficile (CDI), Inflammatory Bowel Disease (IBD), celiac disease and obesity.
Although these are serious health problems, obesity, in recent years has become a global health concern. Even though the exact mechanisms that cause obesity haven’t been identified, recent research shows that gut microbiota plays a crucial role in its onset and progression, and this article will outline some of these factors.
How Changes to the Composition of Gut Microbiota Can Influence Obesity
The composition of the gut microbiota can severely affect an individual’s ability to acquire nutrients and energy. The different species implicated in the progression of obesity include Lactobacillus, Bifidobacterium, Bacteroides, and Enterococcus. The population of microbes in humans is usually stable and homeostasis is maintained to perform essential functions such as metabolism and oxidative phosphorylation.
Homeostasis can be disrupted if the composition of the microbial population changes. For instance, research has shown that in obese patients, the microbiome of the intestine harvests energy more efficiently compared to non-obese patients.
Studies in mice have also shown similar observations whereby a depletion in the Bacteroides species, which includes Bacteroides thetaiotaomicron, is known to protect against the development of adipose tissue i.e., weight gain, was seen in obese mice. Furthermore, it has been suggested that the different composition of gut microbiota can lead to other health problems such as type-2 diabetes.
How Do Antibiotics Affect the Gut Microbiome and Lead To Obesity?
As mentioned previously, antibiotic usage is also a contributing factor to obesity. Since their introduction, antibiotics have become an essential part of day-to-day life. Apart from treating infections, they are heavily present in the environment and production of food as they are part of the diet given to animals that humans consume.
Still, these antibiotics eventually reach humans through consumption and the environment, such as the soil or contamination of water supplies.
Research does not link antibiotic usage directly to obesity but focuses on the alteration of the microbiome, which disrupts homeostasis, which can cause obesity through increased energy usage from the diet. Furthermore, animal studies show that antibiotic exposure reduced populations of bacterial species, such as Lactobacillus and others, related to weight gain.
The mechanisms by which antibiotic exposure occurs are relatively unknown; however, many possible explanations have been proposed, such as some gut bacteria developing the ability to extract more energy and a decrease in bacteria that are thought to protect against the development of obesity.
In terms of human studies and antibiotic exposure, meta-analyses and observational studies of a large group of children reported that when antibiotics were given during the 2nd trimester of pregnancy and infancy, obesity in childhood was observed.
A similar observation was made in adults where treatment with antibiotics caused them to be more prone to weight gain. However, the major limitation of the human studies is that they are all observational, so it is difficult to determine that antibiotic usage is the sole cause of obesity as other environmental factors, such as diet and host genetics, are present.
Influence of Diet on the Microbiome and Obesity
Diet is one of the major factors that can affect the composition of the gut microbiome and increase the risk of developing obesity. Research has shown that when gut permeability is affected, it causes a shift within the bacterial populations leading to inflammation and metabolic disorders linked to obesity.
Additionally, one animal study reported that the consumption of artificial sweeteners could disrupt the microbiota composition within the gut. Here, acesulfame-potassium was given to mice, which altered the gut microbiota leading to weight gain as the pathways that regulate bacterial energy intake were activated.
Obesity continues to be a major health concern, and there are many factors that are intricately linked to its onset and progression. Although the gut microbiome is considered to have a large influence on obesity, it cannot be considered the sole cause. Additionally, a large amount of research is still needed, particularly in humans, to elucidate in detail how the gut microbiota plays a role in regulating human health.
References and Further Reading
Berg, G., et al. (2020). Microbiome definition re-visited: Old concepts and new challenges. Microbiome, 8(1), p. 103. DOI: 10.1186/s40168-020-00875-0.
Davis, C. D. (2016). The gut microbiome and its role in obesity’ Nutr Today, 51(4), pp. 167-174. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5082693/
Del Fiol, F. S., et al. (2018). Obesity: A new adverse effect of antibiotics? Front Pharmacol, 9 p. 1408. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6287021/
Geng, J., et al. (2022). The links between gut microbiota and obesity and obesity related diseases. Biomed Pharmacother, 147 p. 112678. https://pubmed.ncbi.nlm.nih.gov/35134709/
Kho, Z. Y. & Lal, S. K. (2018). The human gut microbiome - a potential controller of wellness and disease. Front Microbiol, 14(9), p. 1835. https://pubmed.ncbi.nlm.nih.gov/30154767/
Vallianou, N., et al. (2021). Do antibiotics cause obesity through long-term alterations in the gut microbiome? A review of current evidence. Curr Obes Rep, 10(3), pp. 244-262. https://pubmed.ncbi.nlm.nih.gov/33945146/
Last Updated: Jun 13, 2023