Before novel therapeutics reach market approval, they must demonstrate their efficacy and safety through rigorous clinical trials. Before this, the pharmaceutical must pass preclinical trials where the drug is tested either in animal models or in human or animal cells in vitro to indicate whether it would likely be worth the time and resources to put the drug through clinical trials.
Here, we discuss the benefits and drawbacks of using animal and human cells for these preclinical trials as well as predict which may be relied upon in the future.

Image Credit: Egoreichenkov Evgenii/Shutterstock.com
Weighing up the benefits: animal vs. human
Preclinical trials take the form of in vitro cell studies or animal studies. Cell studies explore the impact of the novel pharmaceutical on animal or human cells in a lab. Animal studies test the pharmaceutical in vivo in a living creature (not a human), and both methods have benefits and drawbacks.
The most obvious advantage of cell studies is that they do not require living participants. There is no chance of harming a living creature. Additionally, in vitro studies are generally cheaper to set up and run than in vivo studies, and they have a long track record of producing reliable and robust results in relatively short periods.
The greatest limitation of in vitro studies, whether human or animal cell lines are used, is that they cannot recreate the complex environment in which a pharmaceutical compound would be acting. Biological systems are complex; each cell is part of one or multiple pathways and interacts with many other cells, organs, and bodily organisms.
In vitro testing is not yet sophisticated enough to reliably reproduce these complex environments; they can only provide isolated testing environments. So, while in vitro studies offer the huge benefit of testing on human cells without posing an actual risk to humans, they cannot predict the full extent of potential side effects that may emerge the administered to living humans.
On the other hand, in vivo studies test the novel pharmaceutical in a living creature. However, these preclinical studies can only use animals, as safety has not been established to allow for testing in humans. Animal models provide a way of looking at the activity of a drug in complex, biological settings. Some argue that for this reason, animal models can predict the drug’s potential safety profile as they can better demonstrate the complexity of drug activity on living systems.
However, in vivo studies in animals are unreliable in predicting how a drug may impact a human. Animals are different from humans in many ways, and, therefore, the model is not 100% effective at predicting how candidate drugs may affect disease in humans or how they will induce other unwanted effects (known as adverse events).
Overcoming limitations and future directions
While in vitro studies are limited in that they cannot reproduce complex living environments, it is likely that they will continue to be a cornerstone of clinical research. Take the example of oncology research; historically, preclinical cancer trials have generally been ineffective at reliably predicting the therapeutic impact of a novel drug. To overcome this limitation, scientists have been advancing the technology used in these preclinical trials.
As a result, a more complex co-culture technology has emerged. Initial reactions to the technology have been positive, and scientists envision that development of this technology will allow in vitro testing to overcome its limitation of being unable to replicate complex living environments.
Another development in in vitro testing has been adopting 3-dimensional cell culture over 2-dimensional cell culture. This emerging technology has been proven more accurate at replicating the physiologic environment. This technology captures the three-dimensional architecture and heterogeneity of tumor cells in vivo. It remodels the complex micro-environments and surrounding stromal components, helping scientists to explore their drugs in an in vitro environment that more closely resembles an in vivo environment.
In vitro studies have the major drawback of being morally wrong by inflicting pain on animals. There is no way for animal studies to overcome this limitation, and as the world becomes more aware of its sense of responsibility and the virtues of living with morality, it is possible that we will move away from animal studies in the coming years.
While the emphasis will likely move to develop disease models that use animal cells, there will still be development in animal models. New technologies such as CRISPR, for example, will help to make animal studies easier, faster, and more cost-effective.
Overall, there is no clear winner in which model is better at predicting the efficacy and safety of a novel therapeutic. There are those that argue for both sides. However, a growing sense of morality is pushing us to move away from animal models and develop human models so that they can be more effective and reliable.
Bit.Bio, for example, is one company working to make every human cell type available for tests. By doing this, recreating a reliable living system will be easier, and one of the major limitations of in vitro testing of human cells could be overcome.
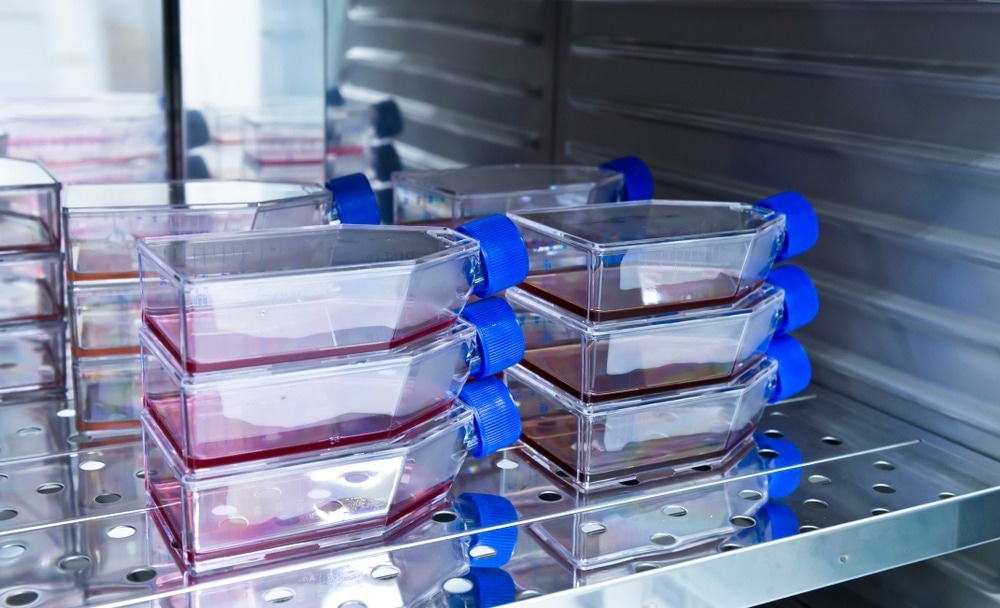
Image Credit: unoL/Shutterstock.com
Sources:
- Arends, M., White, E. and Whitelaw, C., 2015. Animal and cellular models of human disease. The Journal of Pathology, 238(2), pp.137-140. https://pubmed.ncbi.nlm.nih.gov/26482929/
- Focus on a Founder with Mark Kotter| Celebrating 10 years of Community [online]. BitBio. Available at: www.bit.bio/.../focus-on-a-founder-with-mark-kotter-celebrating-10-years-of-community (Accessed April 2022)
- Gargiulo, G., 2018. Next-Generation in vivo Modeling of Human Cancers. Frontiers in Oncology, 8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6192385/
- Højelse, F., 2000. Preclinical Safety Assessment: In vitro - in vivo Testing. Pharmacology & Toxicology, 86, pp.6-7. https://pubmed.ncbi.nlm.nih.gov/10905745/
- Lorian, V., 1988. Differences between in vitro and in vivo studies. Antimicrobial Agents and Chemotherapy, 32(10), pp.1600-1601. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175930/
- Reilly, M. and Rossor, A., 2020. Humans: the ultimate animal models. Journal of Neurology, Neurosurgery & Psychiatry, 91(11), pp.1132-1136. https://jnnp.bmj.com/content/91/11/1132
- Reza Khorramizadeh, M. and Saadat, F., 2020. Animal models for human disease. Animal Biotechnology, pp.153-171. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7329115/
Further Reading
Last Updated: Nov 9, 2022