Alterations in normal RNA splicing patterns have been connected to several different cancer types. While much of this early work has been focused on oncogenic effects that arise due to changes within the splicing reaction, recent studies have dug deeper to determine how mutations within the splicing machinery, particularly splicing factors, may contribute to the progression of various types of tumors and diseases.
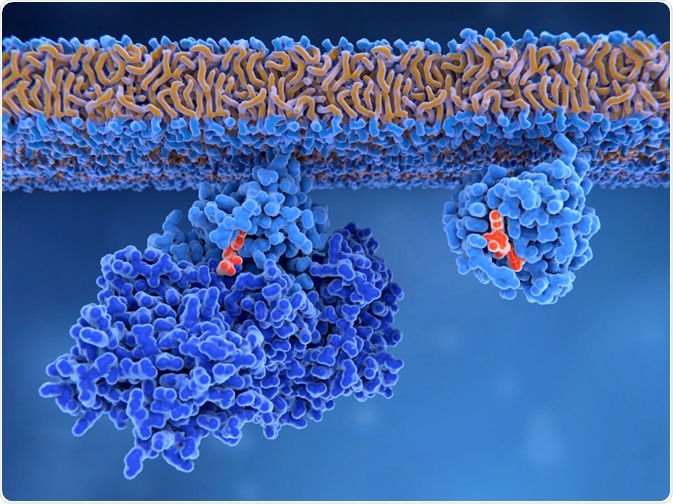
Image Credit: Juan Gaertner/Shutterstock.com
An overview of splicing
The structure of a single strand of RNA includes a single intron with an exon attached on either side. Since introns are non-coding RNA sequences, they must be removed before translation, through a process known as RNA splicing.
Throughout the RNA splicing reaction, several small nuclear ribonucleoproteins (snRNPs): RNA-protein complexes will bind to specific regions of the intron until they undergo a conformational change to become the spliceosome. Once the intron has been cleaved by the spliceosome, the two free ends of the exons are ligated together.
The inclusion or removal of specific exons allows the RNA splicing reaction to play a key role in regulating both the transcription and translation of various components that are essential to maintaining homeostasis to organisms.
Therefore, any type of dysregulation in splicing can inevitably result in a myriad of adverse effects ranging from neurological disorders such as Parkinson’s disease and muscular dystrophy to enhanced tumor development and metastasis in cancer.
Splicing factor mutations
A considerable amount of work published over the past several years has demonstrated that various tumor types exhibit abnormal splicing patterns contributing to their uncontrolled growth.
While this may be true, it was not until recently that researchers have recognized how alterations in the specific components of the splicing machinery may contribute to these tumor-associated splicing changes.
The main structure of the splicing machinery is the spliceosome and its associated splicing factors, which are made up of over 300 proteins and five small nuclear RNAs (snRNAs) that work together to both catalyze and regulate alternative splicing.
During the splicing of RNA, splicing factors function to cleave the intron, ultimately allowing for the exon ends to come together. Any alterations of these splicing factors can contribute to differential splicing patterns that arise in cancerous tissues as compared to that which is present in normal tissues.
The most common splicing factor mutations found in cancers include those involving SF3B1, SRSF2, U2AF1, and ZRSR2.
SF3B1
Splicing factor 3b subunit 1 (SF3B1) is one of the most frequently mutated components of the spliceosome that has been identified in cancerous tissues. Under normal conditions, SF3B1 recognizes the intronic branchpoint sequence (BPS) during the selection of the 3’ splicing site.
Mutations of SF3B1 have been found in several myeloid malignancies, of which its highest occurrence of up to 57% can be detected in patients with myelodysplastic syndromes (MDS).
The hotspots of SF3B1 mutations typically occur on the K700, E622, $625, H662 and K666 genes.
More often than not, the mutations of SF3B1 at these locations are missense substitutions; however, recurrent missense mutations can also occur at these locations. While the presence of SF3B1 mutations is associated with good prognoses in both MDS and uveal melanoma patients, those with chronic lymphocytic leukemia (CLL) have a poor prognosis when SF3B1 mutations are detected.
SRSF2
Following SF3B1, the serine/arginine-rich splicing factor 2 (SRSF2) is considered to be the second-most frequently identified splicing factor mutation. Normally, SRSF2, which is bound to the exon, will recruit U2 small nuclear RNA auxiliary factor (U2AF) upstream to the 3’ splicing site of the intron while simultaneously recruiting U1 snRNP to the downstream 5’ splicing site.
Up to 15% of MDS and up to 50% of chronic myelomonocytic leukemia (CMML) cases are associated with mutations of the SRSF2, which results in a poor prognosis for both diseases.
The contribution of mutant SRSF2 proteins in these diseases is believed to be the result of the unwanted inclusion of a cryptic exon into the mature mRNA that targets the EZH2 protein. By altering the normal reading frame, the EZH2 protein is translated at levels that are much lower than usual.
ZRSR2
In healthy individuals, the zinc finger RNA binding motif and serine/arginine-rich 2 (ZRSR2) will associate with the U2AF heterodimer and contribute to the recognition of the 3’ splicing site by assisting in the formation of the spliceosomal A complex.
In approximately 5% of MDS patients, several different ZRSR2 mutations can arise, which include out-of-frame insertion/deletion, premature stop codon or missense that is distributed along the gene.
One of the major effects that any ZRSR2 mutation can have on splicing is the unwanted retention of U12-type introns, which results in further splicing events that are completely dependent upon the presence of these specific introns.
Interestingly, across most cancer types that have been associated with ZRSR2 mutations, of which include MDS, blastic plasmacytoid dendritic cell neoplasm (BPDCN) and other solid tumors, a strong male predominance has been found.
Conclusion
While a considerable amount of data on splicing factor mutations has contributed to the understanding of how they are related to cancer progression, the precise oncogenic molecular mechanisms behind by these mutations remain poorly understood. Nevertheless, the presence of these mutations is associated with clinical relevance across cancer types.
References
- Koedoot, E., Smid, M., Foekens, J. A., et al. (2019). Co-regulated gene expression of splicing factors as drivers of cancer progression. Scientific Reports 9(5484). doi:10.1038/s41598
- Anczukow, O., & Krainer, A. R. (2016). Splicing-factor alterations in cancers. RNA 26(4); 1285-1301. doi:10.1261/rna.057919.116.
- Bejar, R. (2016). Splicing Factor Mutations in Cancer. RNA Processing; 215-228. doi:10.1007/978-3-319-29073-7_9.
Further Reading
Last Updated: Apr 6, 2020