In prior decades, the pharmaceutical industry has diverted its attention to antibiotic development. Instead, researchers opt to progress treatments for chronic disease.
Unfortunately, the exponential incline in antibiotic resistance was unforeseen, bringing about a very real threat that we are not well equipped to deal with. Because of the rate that binary fission occurs within bacteria, genomic data of archaea and bacteria can alter rapidly in favor of bacterial fitness in a Darwinian nature.
The bacteria that persist against antibiotics do so by altering the drug’s target, or by inhibiting the drug from reaching target sites by ways of efflux pumps, or other physiological adaptations. If left unattended, antibiotics could become moot, and we could all succumb to untreatable infections.
 Biotechnology in the Fight Against Antibiotic Resistance" />
Biotechnology in the Fight Against Antibiotic Resistance" />
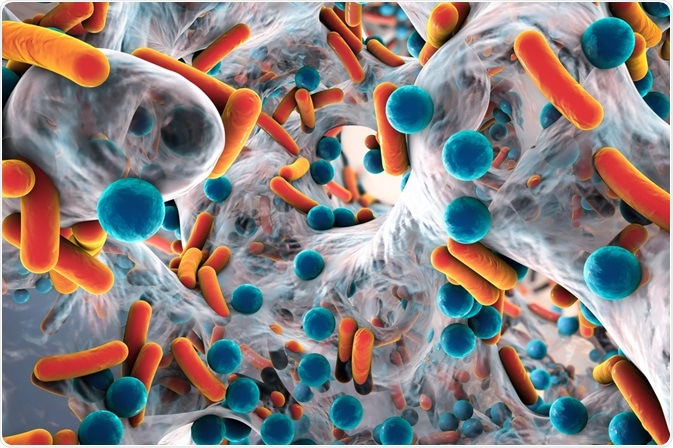
Biofilm of antibiotic-resistant bacteria. Image Credit: Kateryna Kon/Shutterstock.com
The Most Foreboding Bacterial Strains.
The leading antibiotics that are medically available, such as vancomycin, are now being contested by novel strains of bacteria that present a colossal threat. Strains such as methicillin-resistant Staphylococcus Aureus have developed resistance to all antibiotics excluding vancomycin, making it the last line of defense for many strains.
If these strains acquire the ability to resist vancomycin, infectious disease doctors will be ill-equipped, lacking any medicinal remedy in their arsenal to fight off these infections. Other microbial strains such as Enterococcus Faecalis and Enterococcus faecium, have already developed a resistance to vancomycin.
How Bacteria Develop Resistance
Resistance to antibiotics occurs via mutation. For every instance in which bacterial plasmid DNA is expelled in the cytoplasm via mitosis, the genome has the potential to alter. These alterations occur at a rate of 1 in 10 million to 1 in a billion base substitutions per nucleotide per generation. Though this may seem infinitesimal, bacteria procreate exponentially, and those favorable antibiotic-resistant mutations can be transferred with ease from one cell body to another via two core mechanisms.
Transformations could occur, where competent bacterial cells can acquire novel genetic material from their environment, expelled from the remnants of dead bacteria. This single-stranded DNA can invade competent bacterium via the cell membrane upon contact. Because no nucleus is present within bacterial cells, the genomic transcript coalesces with ease.
Even more prominently, conjugation could occur, where this exchange of genes occurs via one live bacterium to another. A donor bacterium can act as a vehicle for a particular DNA sequence, dubbed the F-factor (fertility factor, on a double-stranded plasmid. This “F-factor” is a protuberance in the form of a pilus (a thin tubelike structure). This tool draws both bacteria together, where genetic data is ultimately exchanged to relay this antibiotic-resistant gene.
How are Medical Professionals Tackling These Issues?
With many researchers now geared towards biotechnology and infection, some promising solutions have been brought to the table. Through the exploration of biosynthetic gene clusters (BGCs) from varying bacterial strains, drug discovery could increase exponentially, given that only a segment of bacterial metabolites has been isolated.
Innovative antibiotics of the “glycopeptide” family have garnered interest. These drugs encompass a never-before-seen method of obstructing the bacterial cell wall. Moieties of these compounds bind to the peptidoglycan (a substance forming the cell walls of many bacteria) in a manner that inhibits the activity of autolysins, a set of peptidoglycan-degrading enzymes that bacteria require to remodel their cell wall during growth.
In addition to glycopeptides, Oxazolidinones, (another class of antibiotic), have also been unearthed through the exploration of these BGC’s. Drugs of this kind are used to treat many gram-positive bacteria, which include vancomycin-resistant Staphylococci, Enterococci, and even penicillin-resistant Pneumococci.
Gram-positive bacteria have an archetypal thickness to their peptidoglycan layer, with no outer lipid membrane to protect themselves from cell lysis. Microbiologists are accenting drug development to counter these gram-positive bacteria because this is where the most imminent problems of resistance lie.
The Efficacy of Aminoglycosides
One of the most effective combatants against bacteria, and infection in general, are aminoglycosides. These are a class of antibiotics that inhibits the fundamental bacterial proteins by binding to the 70S ribosomes within the cytoplasm of the cell.
Researchers have already developed self-regenerating aminoglycosides that act as a substrate for resistant enzymes, yielding unstable molecules upon phosphorylation. This phosphate group is abstracted spontaneously, regenerating the original antibiotic in the mechanism below:
Unfortunately, these regenerated aminoglycosides increase the minimum inhibitory concentration (MIC) fourfold. The MIC refers to the lowest concentration an antibiotic can have, whilst still exhibiting the prevention of visible growth of a microbe on agar or in Lysogeny broth (LB) medium. This standard is used to determine whether antibiotics can be used to treat infections while maintaining homeostatic concentration levels in our bloodstream.
Although these self-regenerating aminoglycosides do increase the MIC, this dilemma can be circumvented through the use of drugs such as chlorpromazine, which ameliorate this effect by disrupting aminoglycoside efflux pumps found within the cell walls of many gram-positive bacteria.
Through the biotechnology we currently possess, many of these newfangled methods of antibiotic resistance have been developed, aiding in this war of attrition against microbial organisms. That being said, it is important we do not dither. Alexander Rakwsky, an innovator in the “Division of Anti-infective Drug Products of the FDA”, expresses concern on this scientific front. He claims that with all this attention being diverted to gram-positive, gram-negative bacteria may become resistant from the sidelines of our drug discovery. Resistance is cyclical. The scientific community must always be aware that if you get one class of bacteria under control, any other might sprout from underneath the woodwork to challenge our current medicinal paradigm.
Sources:
- Mao Ye., Mingming Sun., Yanfang Feng., Xu Li., Arthur P. Schwab. Calcined Eggshell Waste for Mitigating Soil Antibiotic-Resistant Bacteria/Antibiotic Resistance Gene Dissemination and Accumulation in Bell Pepper. Journal of Agricultural and Food Chemistry, 64 (27), 5446-5453DOI: 10.1021/acs.jafc.6b00866
- Christian Hobson., Andrew N. Chan., Gerard D. Wright. The Antibiotic Resistome: A Guide for the Discovery of Natural Products as Antimicrobial Agents. Chemical Reviews, 121 (6), 3464-3494, DOI: 10.1021/acs.chemrev.0c01214
- Breijyeh, Z., Jubeh, B., & Karaman, R. (2020). Resistance of Gram-Negative Bacteria to Current Antibacterial Agents and Approaches to Resolve It. Molecules (Basel, Switzerland), 25(6), 1340. https://doi.org/10.3390/molecules25061340
- Domenico Schillaci, Virginia Spanò, Barbara Parrino, Anna Carbone, Alessandra Montalbano, Paola Barraja, Patrizia Diana, Girolamo Cirrincione, and Stella Cascioferro (June 8, 2017) Journal of Medicinal Chemistry 2017 60 (20), 8268-8297 DOI: 10.1021/acs.jmedchem.7b00215
- CELIA M. HENRY Antibiotic Resistance Chemical & Engineering News Archive (2000) 78 (10), 41-58 DOI: 10.1021/cen-v078n010.p041
Further Reading