The brain-gut-microbiome axis constitutes an intricate web of interactions that encompass gut-brain communication, neurotransmitters, microbiota composition and diversity, and even the contribution of probiotics. These elements play important roles in both health and disease. This article provides a comprehensive overview of the current understanding of this complex biological network.
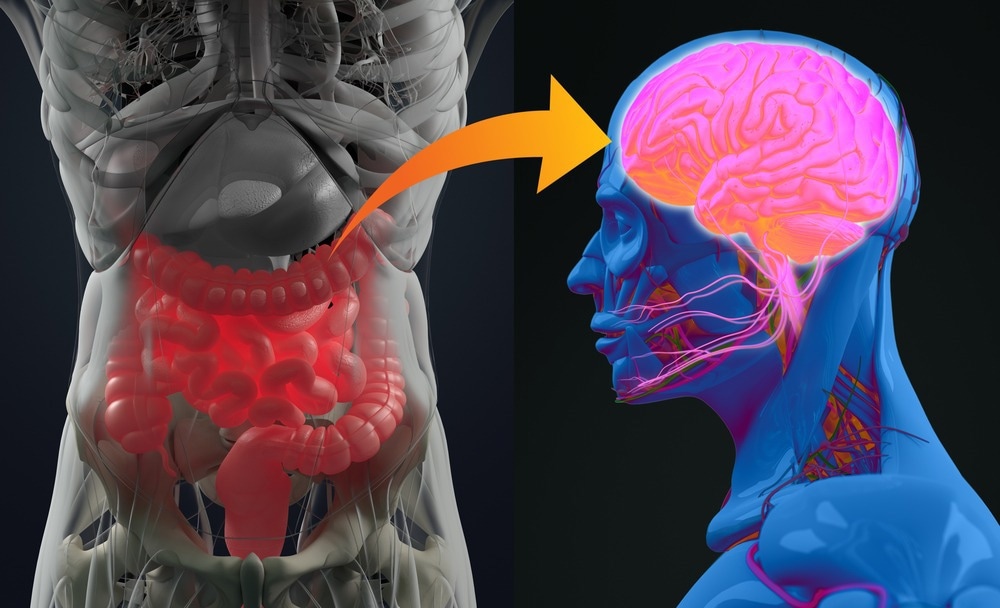
Image Credit: Anatomy Image/Shutterstock.com
What is the Brain-Gut-Microbiome Axis?
Every human has a symbiotic relationship with the microbiome existing in the gut.¹ This microbiome includes trillions of microorganisms in the form of fungi, viruses, parasites, and bacteria.¹ In a normal environment, the microbiome can coexist and generate several benefits to the body.¹ An important link this microbiome has is with the brain, forming what is known as the gut-brain microbiome axis.¹
The axis involves three different systems: the central nervous system, the enteric nervous system, and the gut microbiome.¹ The interaction of these three components can impact various aspects of health, including digestion, mood, mental health, and immunity, through various pathways and molecules, such as hormones, neurotransmitters, cellular activity, and metabolites.¹
The gut-brain-microbiome axis keeps a constant bidirectional communication in response to external and internal signals and changes to try to maintain a balance.² Any perturbation of this balance may result in alterations associated with several diseases.² The high co-morbidity and some psychiatric symptoms (e.g. anxiety, depression) and gastrointestinal problems (e.g. irritable bowel disorder and inflammatory bowel disorder) are clear evidence of the impact that this axis has on the normal function of the body.²
The brain can modulate the activity of the gut through the autonomic nervous system and the hypothalamus-pituitary-adrenal axis, which affects motility, secretion, immune response, and gut permeability.³
Neurotransmitters, short-chain fatty acids, and several other metabolites that can cross the blood-brain barrier from the gut can regulate brain function and behavior.³ Finally, the immune response can be directly affected by the gut microbiome, having a direct impact on the brain and nervous system.³ Also, it can affect the gut-brain axis as a consequence of the environment, diet, and host genetics.³
Recent Breakthroughs in Brain-Gut-Microbiome Axis Research
There are several examples of research studies about the effect of the gut microbiome on the nervous system. Some have focused on the interaction between the brain-gut-microbiome axis on children's neurodevelopment.⁴
For instance, in a study funded by the NIH, 381 children were evaluated, finding that the presence of certain species of microorganisms such as Blautia wexlerae, is associated with greater cognitive development, as well as some others like Ruminococcus gnavus, are more predominant in children with lower cognitive scores.⁴
The researchers focused on the role of the microbiome and how it participated in the metabolism and secretion of neuroactive compounds, which can lead to the development of biomarkers to improve neurocognition and brain health.⁴
Technological Advances in Studying the Brain-Gut-Microbiome Axis
Different techniques have been developed to allow the understanding of this axis. From animal models to bioinformatic tools, all have generated information that helps complete the communication map of this axis, and how it can be improved to benefit health.⁵
Among these techniques are biofabricated gut models, which are in vitro intestinal models that help understand the interactions between the gut microbiome and the nervous system.⁵ 3D modeling of the human brain-gut microbiome axis, germ-free models which can offer information on how the microbiota is a fundamental part of the host's development, especially determining the behavior, physiology, and neurobiology.⁵
Additionally, studying metabolites produced by the interaction of axis components has identified biomarkers that aid in evaluating brain function and their potential role in cognitive disorders.⁵
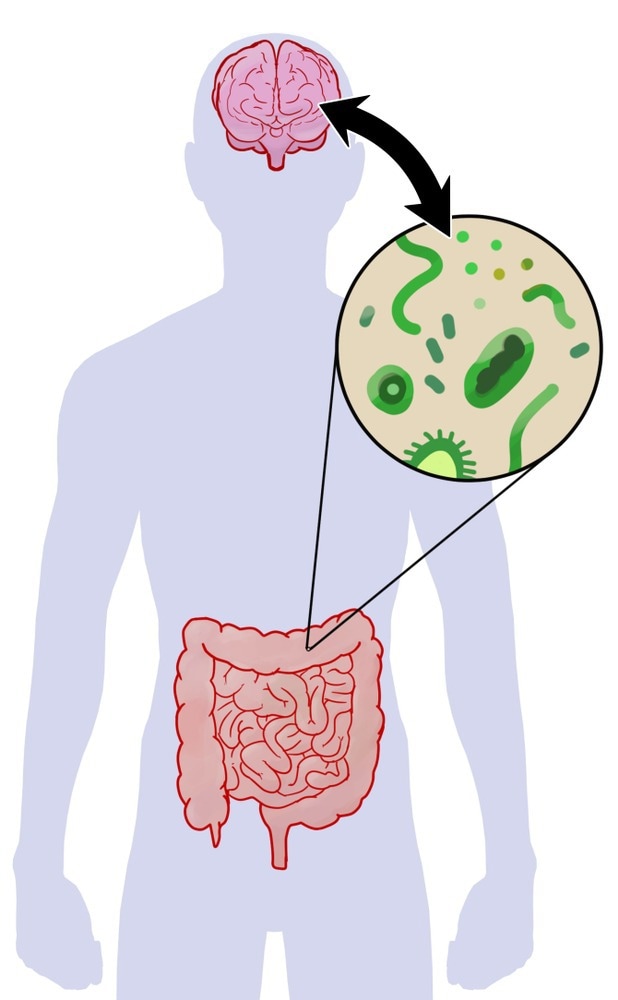
Image Credit: Steven McDowell/Shutterstock.com
Implications for Health and Disease
The brain-gut-microbiome axis participates in numerous processes and is implicated in various diseases, including mental health and mood disorders, neurodegenerative diseases, immune system regulation, obesity, diabetes, and gastrointestinal disorders. Understanding the impact of this axis on different pathologies is crucial for developing effective therapies.⁶
For instance, since the 1980s, researchers have investigated the connection between Parkinson's disease and the gastrointestinal system. They have discovered the presence of alpha-synuclein protein, which is characteristic of the disease and causes the observed effects in patients. According to current theories, the disease may originate in the gastrointestinal system. Changes in the gut microbiota, associated with intestinal inflammation may play a crucial role in the incorrect folding of the alpha-synuclein protein.⁶
Currently, depression is not seen as a disease related only to neurotransmitters; in addition, metabolites and hormones produced in the gastrointestinal tract can interact with the brain and alter its correct functioning.
In a study carried out in Belgium, where stool samples from more than a thousand participants were evaluated, it was possible to differentiate two species of bacteria (Coprococcus spp. and Dialister spp) that were depleted in depressed individuals. Additionally, they found a positive correlation between the ability to synthesize compounds involved in dopamine production and a better quality of life.⁷
Future Directions and Potential Therapeutic Approaches
Continued research is crucial for improving the functioning of the brain-gut-microbiome axis and developing better treatments for associated pathologies. Currently, fecal microbiota transplantation is a therapy used to treat various gastrointestinal disorders. It works by transferring feces from healthy to affected patients.⁵
It has been reported that probiotics can fight some infections and have cognitive and emotional effects. Strategic diets that include probiotics, prebiotics, and fiber-rich foods can improve the composition and diversity of the microbiome by providing the necessary components to promote the growth of beneficial microorganisms.⁵
Ultimately, it is important to note that preserving efficient brain-gut communication is key in maintaining good cognitive and gastrointestinal health, and preventing several diseases. This can be accomplished by stimulating the vagal nerve, utilizing immune system-promoting components, and employing microbiome metabolites. Microbiome-targeted drugs may also be used to enhance the effect on the axis.⁵
Sources:
- Milestones in human microbiota research. (2019, June 18). Nature. [Online]. Available at: https://www.nature.com/collections/microbiota-milestone
- Cryan, J. F., et al. (2011) The microbiome-gut-brain axis: from bowel to behavior. Neurogastroenterology & Motility, 23(3), pp. 187–192. doi.org/10.1111/j.1365-2982.2010.01664.x
- Martin, C. R., et al. (2018) The Brain-Gut-Microbiome Axis. Cellular and Molecular Gastroenterology and Hepatology, 6(2), pp. 133–148. doi.org/10.1016/j.jcmgh.2018.04.003
- Wang, Q., et al. (2023) The microbiota–gut–brain axis and neurodevelopmental disorders. Protein & Cell, 14(10), pp. 762–775. doi.org/10.1093/procel/pwad026
- Hall, V., et al. (2023) Getting closer to modeling the gut-brain axis using induced pluripotent stem cells. Frontiers in Cell and Developmental Biology, 11. doi.org/10.3389/fcell.2023.1146062
- Mehanna, M., et al. (2023) Study of the gut microbiome in Egyptian patients with Parkinson’s Disease. BMC Microbiology, 23(1). doi.org/10.1186/s12866-023-02933-7
- Valles-Colomer, M., et al. (2019) The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology, 4(4), pp. 623–632. doi.org/10.1038/s41564-018-0337-x