Cryoprecipitate Is a substance produced due to the gradual thawing of Fresh Frozen Plasma (FFP). Gradual thawing causes the precipitation of proteins rich in fibrinogen, factor VIII, von Willebrand factor, fibronectin, and factor XIII. Cryoprecipitate is considered a plasma product and is subject to the same compatibility as normal blood (ABO).

Image Credit: Ormalternative/Shutterstock.com
In the clinical setting, cryoprecipitate is used to replace fibrinogen. As with fresh frozen plasma, the plasma from which the cryoprecipitate is produced has been subject to leukocyte depletion and is typically obtained from a male donor, as this reduces the risks of transfusion-related acute lung injury (TRALI).
What Is Cryoprecipitate Composed Of?
Cryoprecipitate principally contains fibrinogen and high concentrations of factor VIII. It also contains lower concentrations, including factor XIII, von Willebrand factor, fibronectin, and platelet microparticles. Due to differences in the manufacturing process and blood donor variability, the concentration of each component varies in cryoprecipitate. However, some blood transfusion services stipulate a minimum concentration of each component per unit of cryoprecipitate. The main component of focus is fibrinogen. The minimum requirements for each component in cryoprecipitate for therapy are as follows:
- Fibrinogen: minimum specification of 140mg/U (the standard adult dose is 10U)
- Factor VIII: mean concentration of 101 IU/U (minimum specification 70 IU/U)
- Fibronectin: 1500 mg/mL (normal plasma levels are 300 mg/mL)
- Factor XIII: ~ 20–30% original factor XIII of plasma; 223 fold higher than fresh frozen plasma
- von willebrand factor: ~80–100 IU/U (~40–70% original von willebrand factor in original plasma)
- Platelet microparticles: 256 times greater than source plasma
Why Is Fibrinogen Important?
Fibrinogen is essential for hemostasis – a process to prevent and stop bleeding. The liver produces fibrinogen in the body, which serves as the most abundant coagulation factor in blood plasma. It is a dimeric protein comprised of three pairs of polypeptide chains. After the tissue is injured, thrombin cleaves fibrinopeptide chains To yield fibrin monomers. These subsequently joined together to form insoluble fibrin polymers.
Alongside this, thrombin activates factor XIII, which binds and crosslinks the fibrin strands. This results in the stabilization of the clot and decreases the probability that the clot will be degraded as a consequence of crosslinking fibrinolytic inhibitors (namely α2-antiplasmin) into the fiber network. Fibrinogen also binds fire receptors on the platelet membrane; this serves to promote the aggregation of platelets and causes them to localize at the site of the developing clot.
What Is Cryoprecipitate Used For?
Originally, cryoprecipitate was developed as a therapy for patients who suffered from antihemophilic factor deficiency or hemophilia. This therapy has been in use for over 50 years. Since its inception, however, cryoprecipitate use has extended beyond its original purpose and is more commonly used to replenish fibrinogen levels in patients.
Currently, cryoprecipitate is the only satisfactory fibrinogen concentrate available for intravenous use. Cryoprecipitate has two clearly defined clinical indications: the treatment of hemophilia on supplementation of fibrinogen (as a consequence of inherited and acquired disease).
However, the way that cryoprecipitate is used worldwide tends to vary due to differences in licensing. Cryoprecipitate is produced in the USA, Canada, United Kingdom, Australia, and New Zealand, where it is principally used for acquired hypofibrinogenemia.
Outside of these countries, cryoprecipitate production has been phased out in favor of fibrinogen concentrate for congenital and acquired deficiencies in fibrinogen.
The clinical indications for cryoprecipitate in adults occur in cases where fibrinogen levels are depleted, and fibrinogen levels decreased to a critical level. These are in cases of coagulopathy (bleeding disorder) where clinically significant bleeding occurs, which results in a fibrinogen level of < 1.5g/L (or < 2g/L in cases of obstetric bleeding). Cryoprecipitate may also be used when fibrinogen levels fall below 1g/L. When bleeding is associated with thrombolytic therapy, and in cases of inherited hypofibrinogenemia, fibrinogen concentrate is unavailable.
Cryoprecipitate is a pooled product, and its use has been associated with several adverse events. Most notably is the transmission of bloodborne pathogens and TRALI.
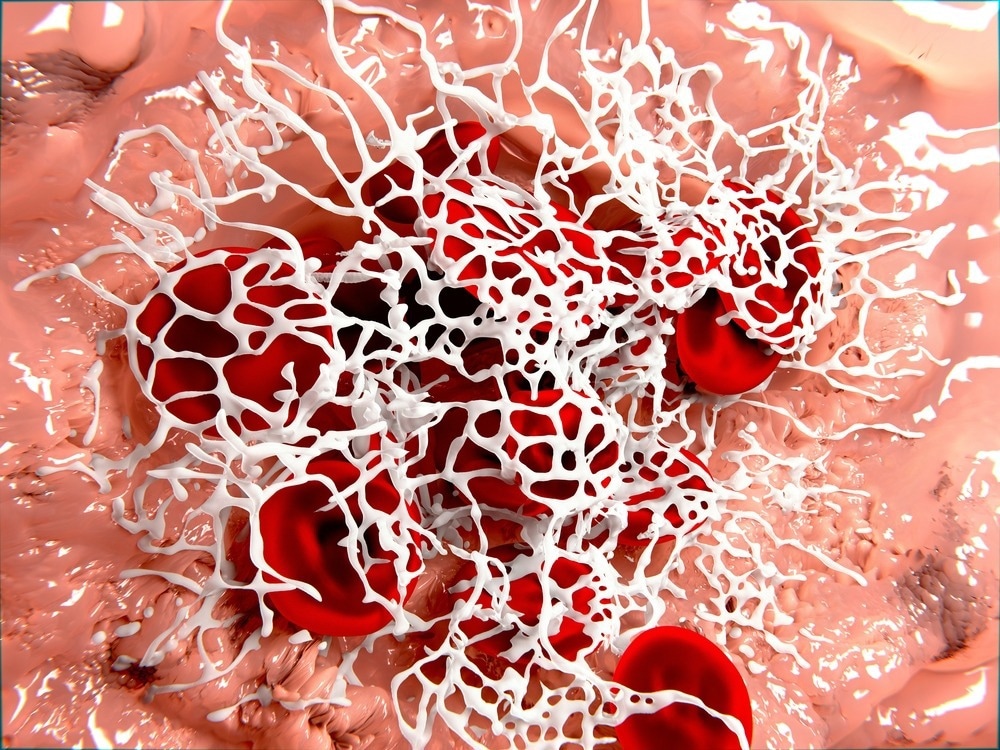
Image Credit: Juan Gaertner/Shutterstock.com
The Safety of Cryoprecipitate Therapy
Cryoprecipitate has been used for over 50 years. The literature has documented a few adverse events related to cryoprecipitate therapy. However, this pause in the team of safety events may reflect a lack of data collection, reporting bias, as well as definitive low risk from its use. The principal concern related to safety is the risk of viral transmission, particularly as it does not undergo pasteurization or viral inactivation.
To reduce the likelihood of pathogenic consequences, cryoprecipitate is treated with riboflavin and ultraviolet light; alternatively, amatosalen, ultraviolet light, and solvent detergent filtration have been employed. These, however, have been met with limited success - as these tend to compromise the fibrinogen content, reducing it by an average of ~ 30%.
The UK haemovigilance scheme, Serious Hazards of Transmission (SHOT), has analyzed data between 1996 and 2014 and reported no cryoprecipitate-related viral transmission cases were reported in this timeframe. Over this same time frame, SHOT reported five cases of viral transmission with fresh frozen plasma. Recommendations from the 2014 SHOT report stated that female-derived donor plasma should be avoided in the production of cryoprecipitate as in this., there was a documented case of TRALI. However, there was a low incidence of acute transfusion reactions (1 out of 43 transfusion reactions was attributed to cryoprecipitate).
Another important adverse outcome to consider when administering cryoprecipitate is the risk of thrombotic events, as high fibrinogen levels are a known risk factor for this. Literature has documented that patients who received large volumes of transfusion therapy, which include cryoprecipitate, as well as prohemostatic agent, for major hemorrhage, are at an increased risk of thrombosis.
Despite this correlative relationship, data from the CRYOSTAT randomized controlled trial, which evaluated cryoprecipitate in trauma hemorrhage, showed no difference in fibrinogen levels 24 hours and up to 28 days after treatment. Moreover, thrombotic events were only demonstrated in the cohort that had received standard treatment, not in the early cryoprecipitate cohort.
The most recent data has also demonstrated that no thrombotic or safety concerns with fibrinogen concentrate have been observed.
Cryoprecipitate has been used for over 50 years, with very few instances of viral transmission or other adverse complications. It should be noted that this may be due to a lack of reporting. However, many countries worldwide have replaced cryoprecipitate in favor of fibrinogen concentrate. It offers the advantages of additional safety measures for reducing viral transmission, increased amenability to transport, and near-patient availability. However, recent preclinical studies have demonstrated the stability of fibrinogen in authority cryoprecipitate; this positions cryoprecipitate as a more rapidly available source for transfusion.
The discrepancy in the licensed indication for cryoprecipitate indicates gaps in knowledge. In addition, the Effect of the other components found in cryoprecipitate is unknown but thought to have a major effect on hemostasis. Literature anticipates significant growth in understanding of cryoprecipitate as several prospective studies investigating whether the additional proteins in cryoprecipitate confirm any hemostatic benefit in different types of bleeds are being conducted. This may have important implications as the treatment of major hemorrhage is moving beyond generic to a more individualized approach.
Sources:
- Holcomb JB, Fox EE, Zhang X, et al. (2013) Cryoprecipitate use in the PROMMTT study. J Trauma Acute Care Surg. doi:10.1097/TA.0b013e31828fa3ed.
- Wong H & Curry N. (2016) Cryoprecipitate transfusion: current perspectives. International Journal of Clinical Transfusion Medicine. doi: 10.2147/IJCTM.S99042.
- Bolton-Maggs PHB, Poles D et al On Behalf of the Serious Hazards of Transfusion (SHOT) Steering Group. The 2014 Annual SHOT Report. Manchester, UK. 2015.
- Curry N, Rourke C, Davenport R, Beer S, et al. (2015). Early cryoprecipitate for major haemorrhage in trauma: a randomised controlled feasibility trial. Br J Anaesth. 2015 doi: 10.1093/bja/aev134.
Further Reading