T cells are a type of immune system cell. There are three general types of T cells, regulatory T cells (Treg cells), cytotoxic T cells and T helper cells. T regulatory cells suppress potentially harmful actions of T helper cells.
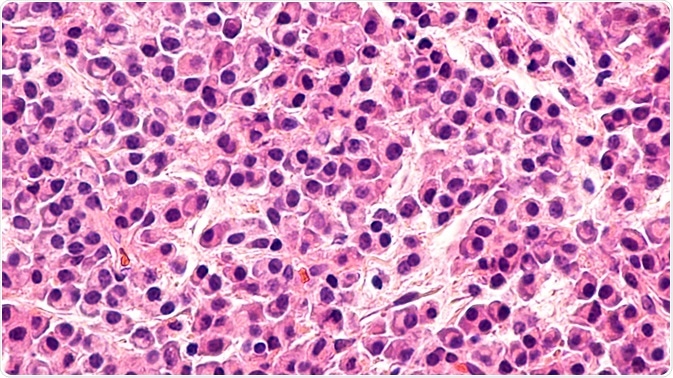 Credit: David Litman/Shutterstock.com
Credit: David Litman/Shutterstock.com
Some functions of T regulatory cells include:
- Preventing autoimmune disease
- Suppressing allergies and asthma
- Mediating maternal-fetal immune tolerance
- Regulating oral tolerance
- Suppression of pathogen-induced immunopathology
- Suppression of T-cell activation by weak stimuli
- Control of magnitude of immune response by T helper cells
- Protection of commensal bacteria
Types of Treg cells
A number of subpopulations exist within Treg cells. Some of the best characterized of these express CD4, CD25 and FOXP3. Natural Treg cells account for between 5 and 10 percent of all CD4+ helper inducer T cells. They have intermediate to high expression of the IL-2 cell surface receptor and intracellular expression of the transcription factor FoxP3.
Tr1 cells produce large quantities of IL-10 and smaller amounts of IL-3, but do not produce IL-4. Tr1 cells are involved in induction of tolerance to self and tolerance of non-harmful foreign antigens, such as food antigens. They inhibit proliferation and cytokine production of effector T cells.
Th2 cells resemble Tr1 cells, but are modulated by TGF-β. They help with IgA synthesis and chemotaxis of leukocytes, and have properties for suppressing other immune cells. TGF-β is important for maintaining tolerance in mucosal surfaces. An example is oral tolerance.
Development of Treg cells
T cells are made in the bone marrow, and committed to a specific lineage in the thymus. All begin without CD4 and CD8 surface proteins. These are known as CD4-CD8-, or double negative (DN) cells. At this stage, the cell rearranges its genes to for a unique molecule that can be tested against cells in the thymic cortex for interactions with self.
T cells that test positive proliferate and begin expressing CD4 and CD8, and are known as double positive cells. Double positive Treg cells are selected based on interaction with other cells in the thymus. They begin transcribing FOXP3 and become mature Treg cells.
Preventing autoimmunity
Treg cells develop in the thymus and are released upon stimulation by chemokines released from a site of injury or inflammation. The cells migrate to the site and nearby lymph nodes. There, immunosuppression results from direct interactions with effector cells.
Treg cells can downregulate activities of autoreactive T cells, such as activation and clonal expansion. They induce and maintain immune tolerance through recognition of autoantigens from the injured tissues. The subsequent immune response can be modulated through cell-to-cell contact or soluble cytokines.
Treg cells also have cytotoxic activity. Its target cells include CD4+ and CD8+ T cells, NK and NKT cells, monocytes, dendritic cells, and granulocytes. Tregs have the ability to restrict CD8+ memory effector T cells.
A balance between activated and effector Treg cells is necessary for a proper immune response. Increases in Treg cells may be helpful for autoimmune disease and allergies, as well as prevention of graft rejection. Conversely, decreasing Treg cells could improve immunity against tumors and pathogens.
Further Reading