Macrophages are vital cells in the inflammatory response to wounds or infections. They have several roles in inflammation, including clearing necrotic debris and pathogens, reducing inflammatory levels after an infection has cleared, and repairing damaged tissue.
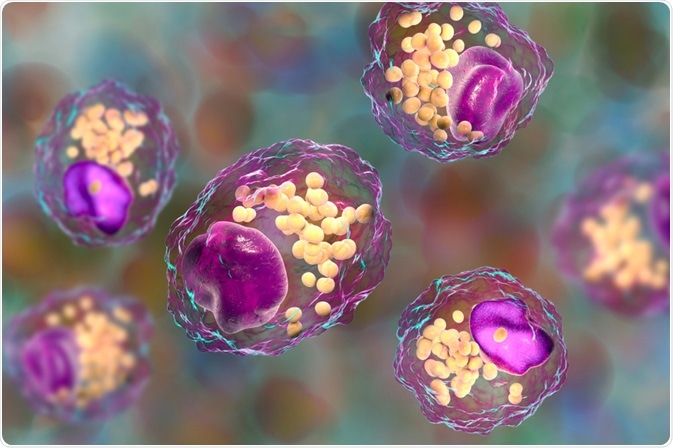
Macrophage Cells. Image Credit: Kateryna Kon/Shutterstock.com
To have this range of functions and mechanisms, macrophages differentiate into a variety of subtypes. These subtypes are not easily defined but range from M1 to M2 at either extreme. Differentiation into these subtypes is known as polarization and occurs as a response to the macrophage’s microenvironment.
Macrophages and their roles in infection response
M1 macrophages are pro-inflammatory. They are the primary line of defense against intracellular pathogens like viruses and some bacteria and are crucial in the activation of CD4+ T cells. They are characterized by varying levels of presentation of CD64 and CD80 surface antigens, as well as their induction of acute inflammation by the production of pro-inflammatory cytokines.
These cytokines include a range of interleukins, interferon, and tumor necrotic factor, as well as a wide variety of chemokines. These chemokines, including members of both the CXC and CCL families, induce the chemotaxis of phagocytes, including neutrophils, mast cells, and dendritic cells, as well as both other macrophages and undifferentiated monocytes.
The combination of cytokines, particularly the high concentrations of interleukin 12, produced by M1 macrophages also induces differentiation of T helper lymphocytes into Th1 cells. Due to this association, both M1 macrophages and Th1 lymphocytes are involved mainly in intracellular infections. M1 macrophages, in addition to aiding inflammation, are heavily involved in phagocytosis of pathogens and dead or damaged tissue from infection or injury.
At the other end of the spectrum of macrophage functions, M2 macrophages are those involved in tissue repair. They are identified by their expression of different surface antigens, known as CD11b and CD209. Like M1 macrophages, M2 macrophages help remove dead and damaged cells, though they are not involved in phagocytosis of pathogens. M2 macrophages produce very low quantities of some pro-inflammatory cytokines, such as interleukin 12, however, these are negligible compared to the anti-inflammatory cytokines that they produce.
The main anti-inflammatory cytokine produced by all variations of M2 macrophages is interleukin 10. Interleukin 10 acts as an antagonist to many pro-inflammatory signals, as well as being involved in T cell regulation. It has been shown to inhibit the pro-inflammatory Th17 subset of T lymphocytes, as well as upregulating Tregs, the regulatory and anti-inflammatory subset of T lymphocytes.
Due to their role in damage limitation and repair, M2 macrophages are involved in later stages of the inflammatory process, and their differentiation is induced by signals that are more prevalent several hours or even days after infection.
Polarization signals
Macrophages are highly plastic cells that develop from monocyte progenitors. Monocyte progenitor cells mature into monocytes in the bloodstream, then mature further into macrophages, interstitial dendritic cells, or microglial cells when progressing into tissue.
Monocyte maturation into either M1 or M2 macrophages depends on the environment within the tissue, and even once differentiated, macrophages can change their function and phenotype due to their innate plasticity. Macrophages are also able to possess characteristics of both M1 and M2 subsets, hence the existence of macrophages on a spectrum and frequent use of the terms ‘M1-like’ and ‘M2-like’ macrophages.
Macrophage differentiation into M1 or M1-like macrophages is prevalent within the early stages of inflammation and is induced in environments containing high levels of Toll-like receptor and interferon signaling. In vitro, M1 polarization is induced by the use of granulocyte/macrophage colony-stimulating factor (GM-CSF), as well as type 2 interferon and Toll-like receptor agonists.
In vivo, the polarization of macrophages into M1 type is frequently due to the expression of interferon-gamma, a type 2 interferon, by nearby Th1 cells, which are highly prevalent in inflammatory microenvironments. These signals induce the appropriate surface protein expression by the macrophage and therefore its polarization towards M1. M1 cells further induce Th1 differentiation, causing an amplification in both Th1 and M1 cells in inflammation.
Macrophages differentiate into M2 macrophages as a result of different signaling factors. These include interleukins 4, 10, and 13, as well as macrophage colony-stimulating factor (M-CSF). Not all signals are required to induce polarization, though in vivo there is generally a combination of different interleukins in the surrounding environment. These signals are all produced by Th2 subtype T lymphocytes, meaning that M2 macrophages are more prevalent in parasitic and other extracellular infections.
In vitro, M2 polarization is induced via M-CSF. It has been shown that stimulation via GM-CSF and M-CSF can induce polarization towards M1 and M2 respectively even on macrophages that are already polarized, though it is common for the macrophages to retain some characteristics, such as varying phagocytic abilities.
The ability of macrophages to polarize in this highly plastic manner is crucial in allowing the immune system to adapt to varying threat levels from microbes and the resulting tissue damage, thus allowing infections to fully resolve.
References
- Atri, C., Guerfali, F. Z. and Laouini, D. (2018) ‘Role of human macrophage polarization in inflammation during infectious diseases.’ International Journal of Molecular Sciences.
- Murray, P. J. (2017) ‘Macrophage Polarization.’ Annual Review of Physiology.
- Oishi, Y. and Manabe, I. (2018) ‘Macrophages in inflammation, repair, and regeneration.’ International Immunology.
- Tarique, A. A., Logan, J., Thomas, E., Holt, P. G., Sly, P. D. and Fantino, E. (2015) ‘Phenotypic, functional, and plasticity features of classical and alternatively activated human macrophages.’ American Journal of Respiratory Cell and Molecular Biology.
- Wei, H., Li, B., Sun, A. and Guo, F. (2019) ‘Interleukin-10 family cytokines immunobiology and structure.’ In Advances in Experimental Medicine and Biology.
Further Reading
Last Updated: Dec 15, 2020