Metastasis refers to the spread of cancer cells from primary tumors to distant sites that they then colonize to form a metastatic tumor.
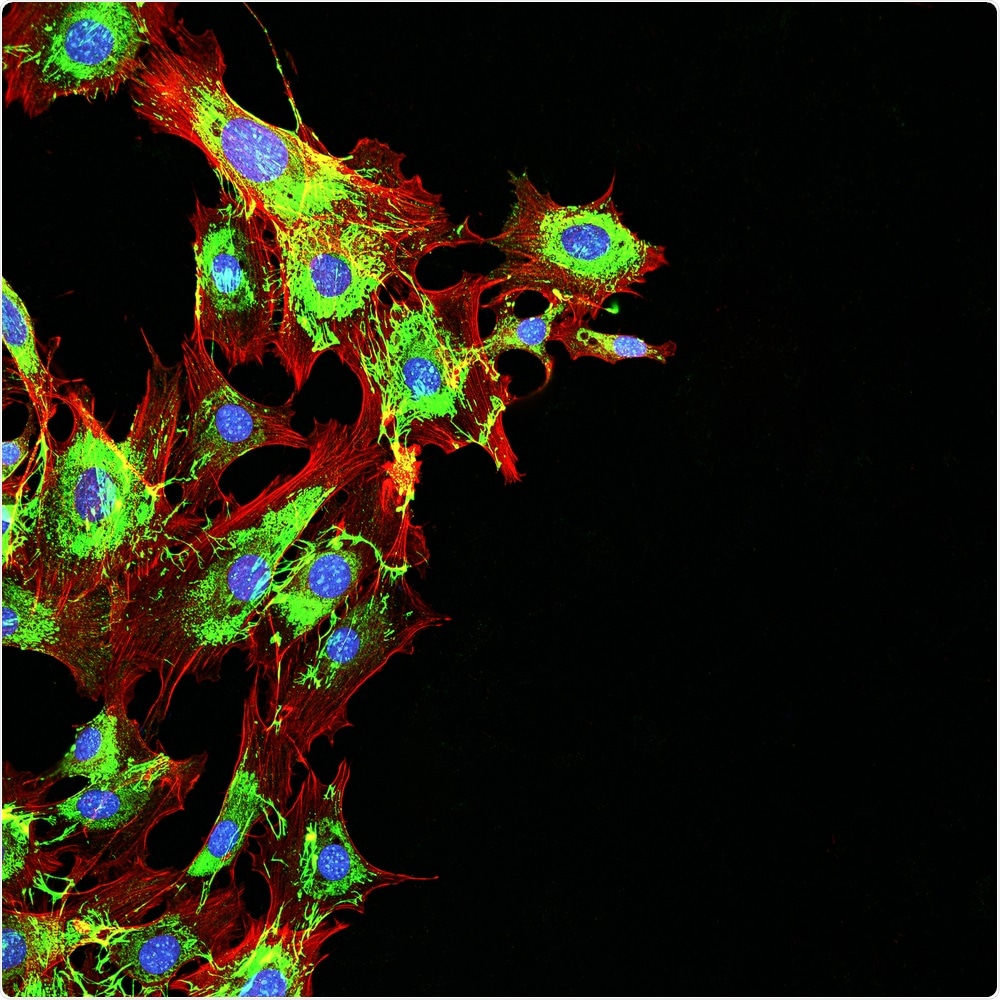
Image Credit: DrimaFilm/Shutterstock.com
Although researchers have made excellent progress in understanding primary tumors, survival rates among patients with metastatic cancer are poor, with metastatic cancer accounting for 90% of cancer-related deaths.
About the metastatic process
Research has shown that the metastatic process is inefficient, with most cancer cells getting lodged in capillaries and dying within 24 hours of entering the bloodstream. Furthermore, cancer cells that do reach distant sites in the body rarely form macrometastatic tumors.
Cancer cells are not positively selected for metastasis. Instead, they probably possess genomic features and key driver adaptations that may get selected to improve their chances of acquiring traits such as immune evasion and survival in the bloodstream.
This “metastatic potential” is unlikely to be confined to the cancer cells themselves. Rather, it depends on complex cancer cell-host interactions.
Traditionally, metastasis had been considered an end-result of cancer development, but emerging data increasingly points towards early and late metastatic dissemination and both monoclonal and polyclonal seeding patterns.
Now, Nicolai Birkbak (Department of Molecular Medicine, Aarhus University, Denmark) and Nicholas McGranahan (University College London Cancer Institute) have provided a comprehensive overview of cancer genome studies looking at the differences between metastatic and primary tumors, the genomic drivers of metastasis and the different modes of metastatic spread.
Drivers of metastasis
Writing in the journal Cancer Cell, the reviewers begin with a description of the genomic landscape of metastatic cancer. They explain that key alterations that arise in metastatic cancer cells are not simply metastatic mutations but have probably been acquired by ancestrally “normal” cells or by an ancestral primary tumor cell or metastatic cell.
However, most of the alterations will be “passengers,” with only a few being the drivers that promote cancer cell fitness.
The clinical relevance of these driver alterations and cancer cell fitness has been demonstrated – therapies designed to target driver events often result in cancer regression. However, in the case of metastasis, this is often only temporary.
Furthermore, studies of these driver alterations have generally been focused on primary cancer, meaning many questions remain about metastatic cancer cell genes and driver events.
The two main genomics research approaches
The reviewers discuss the two main approaches that have been used to determine genomic features in metastatic cancer and the associated genes and driver alterations.
One main approach is the large-scale cohort analysis of metastatic samples, where genes commonly mutated in cases of metastasis as well as mutations in cancer-associated genes of the primary tumor are studied.
Such studies have tried to identify drivers of metastasis but, according to Birkbak and McGranahan, so far there has been a “conspicuous absence of cancer genes exclusively mutated in the context of metastatic disease have been identified.”
The reviewers say one study identified a long-tailed distribution of cancer driver alterations but that none were found to be specific to metastasis. Larger scale panel-based and whole-genome sequencing studies of various cancer types have generated similar findings.
However, ongoing large-scale studies such as the multi-year AACR Project Genomics Evidence Neoplasia Information Exchange (GENIE) initiative aims to analyze thousands of both primary and metastatic cancer samples to provide data that is easily accessible to researchers.
Large-scale genomics studies of metastasis have found that metastatic cancer samples generally demonstrate a higher mutation burden and more driver events and aneuploidy than primary cancer samples.
However, researchers have still been unable to identify commonly shared events that may confer metastatic potential. However, the specific drivers of metastasis may still be identified through approaches that also consider system-level changes such as the timing of dissemination and transcriptional changes.
The other main approach to determine genomic features in metastatic cancer that the reviewers discuss is a paired analysis of primary-metastatic samples.
This can potentially determine whether one biopsy taken from a primary tumor or metastatic cancer is enough to guide therapeutic decision making. Furthermore, by identifying events that are enriched at sites of metastasis, this approach can distinguish between specific events that occurred before or after metastatic dissemination.
The reviewers say that, overall, the data support that cancer progression is characterized by the high-acquisition of cancer-specific driver events that early on in disease that tend to be found clonally in primary tumors.
The clonal nature of these events means they can reliably be identified in biopsies taken either from primary or metastatic tumors.
However, it also appears that most solid tumors undergo subclonal divergence, says the team, and future studies should investigate the long tail of subclonal drivers in terms of both the biological and clinical perspectives.
Considering the mode of metastatic dissemination
Birkbak and McGranahan go on to discuss the modes of metastatic dissemination, including monoclonal and polyclonal dissemination from the primary tumor.
Monoclonal dissemination refers to the acquisition of metastatic potential in a single subclone within the primary tumor and subsequent seeding of all metastatic lesions, while polyclonal dissemination refers to acquisition in many different subclones that results in the seeding of one or more metastatic lesions.
Studies demonstrating the heterogeneity and branched tumor evolution in primary tumors raise questions about whether metastasis is seeded by one subclone in one branch of the phylogenetic tree or many subclones on different branches.
The authors also touch on the role that the timing of metastasis plays. Although traditionally, metastasis was considered as an end-result of cancer progression, reports have suggested that dissemination can occur early in the course of the disease and that primary and metastatic tumors develop simultaneously.
Given the major clinical implications of early versus late metastatic dissemination, methods that detect disease at the time of diagnosis are urgently needed. Approaches that use circulating tumor DNA (ctDNA) for early diagnosis of regression have proved successful over recent years, but the sensitivity of these approaches needs improving.
“Nevertheless, as the technology matures and enters clinical practice, increased sensitivity may present ctDNA assays as an excellent tool to supplement diagnostic imaging to detect early metastatic spread and guide treatment choices,” suggest the reviewers.
The reviewers go to discuss the role that the immune micro-environment might play in shaping cancer metastasis genomics and refer to a study that reported a loss of heterozygosity (LOH) at the human leukocyte antigen (HLA) loci during the metastatic transition. They suggest that a more holistic view that goes beyond the exploration of genomic evolutionary trajectories is needed to fully understand the metastatic disease.
Our knowledge about cancer genome evolution is “only in its infancy”
In their final comments, Birkbak and McGranahan say “our knowledge of the cancer genome evolutionary trajectories of metastasis is only in its infancy.”
A more comprehensive picture of the landscape of metastatic disease, is needed, they say, and comprehensive sampling of primary and matched tumors is needed to characterize the prevalence and importance of different modes of metastasis.
Such detailed cartography of metastasis is required to inform clinical decision making and create new therapeutic opportunities,”
Journal references:
Birkbak N and McGranahan N. Cancer Genome Evolutionary Trajectories in Metastasis
Cancer Cell 2020;37(1): p8 to 19:https://doi.org/10.1016/j.ccell.2019.12.004