Lipids generated by the body’s insulin-producing beta cells in the pancreas can cause the cells' own death are the conclusions drawn by a team of scientists from the University of Alabama at Birmingham and the University of South Florida.
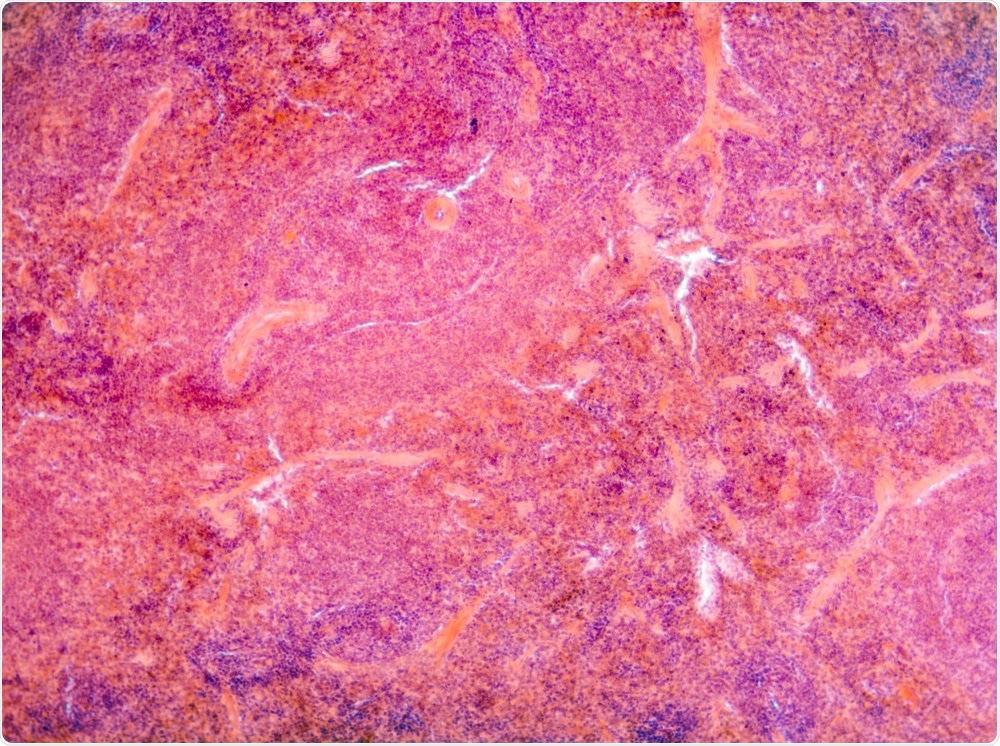
Image Credit: Pan Xubin/Shutterstock.com
In a paper published in the Journal of Lipid Research last December, the researchers outline how these findings will be relevant to the treatment of Type 1 diabetes and may lead to improved strategies to prevent or delay the initiation of the disease.
What forces macrophages into its distinct phenotypes?
In autoimmune diseases, a continued inflammatory response continues can lead to significant tissue and organ damage as the immune cells attack the body’s cells. In the case of Type 1 diabetes, the immune system’s macrophages and T cells attack the insulin-producing beta cells found in the pancreas. Over time, the death of these cells causes the body’s insulin levels to drop, and potentially, completely diminish.
For the past several decades, Dr. Sasanka Ramanadham has been studying lipid signaling in Type 1 diabetes at the University of Alabama. Meanwhile, at the University of South Florida, Dr. Charles Chalfant has been investigating lipid signaling in cancer.
For both groups of studies, Chalfant provides expertise in mass spectrometry which is used to identify and quantify the lipids found in the different samples.
It is already known that the immune system has two different phenotypes of macrophage cells that work antagonistically. The first, M1 cells, initiate phagocytosis to attack infections, as well as by increasing inflammation as a response to secretion signals. M2 cells, on the other hand, work to reduce inflammation and repair tissue damage.
In the current study, scientists aimed to uncover how signaling forces these macrophage cells into either one of these two phenotypes. Gaining an understanding of how M1 cells are activated in Type 1 diabetes would be relevant to establishing new strategies to delay or even prevent the disease from developing.
Investigating the M1 and M2 phenotype expression
The Ca2+-independent phospholipase A2beta, or iPLA2beta, was the enzyme focussed on in the study. It was chosen because it is known for its role in hydrolyzing membrane glycerophospholipids within the cell membrane, resulting in the release of a lysophospholipid and a fatty acid, which then go on to modulate cellular responses.
Other enzymes are then enlisted to transform these fatty acids into bioactive lipids, which the Ramanadham determined as iPLA2beta-derived lipids or iDLs. Research has shown that these iDLs can have a pro-inflammatory effect via promotional the M1 macrophage phenotype, or, they can have a pro-resolving impact via the promotion of the M2 macrophage phenotype.
The type of phenotype that is expressed is dependent on which pathway is most active. Also, the iDLs are then released by the cell, meaning that they could be involved also in cell-to-cell signaling.
It has been found that iPLA2-beta activity is expressed by beta cells and macrophages. To investigate how iDLs could impact inflammation, the team compared iPLA2beta-knockout mice with mice whose beta cells had been engineered to over-express iPLA2beta.
The scientists isolated macrophages from the iPLA2beta-knockout mice and activated them to induce the M1 phenotype. Then, the iDL eicosanoids that had been generated by the macrophages that lacked iPLA2beta were measured. In comparison with the wild type activated macrophages, there were lower levels of production of pro-inflammatory prostaglandins by the knockout macrophages along with an increased level of resolvin D2, a specialized pro-resolving lipid mediator. These results provided evidence of the M2 phenotype which produces a reduced inflammatory state.
On the other hand, the macrophages that were studied from the mice whose beta cells were engineered to over-express iPLA2beta demonstrated increased production of pro-inflammatory eicosanoids as well as reduced levels of resolvin D2. This demonstrated the expression of the M1 phenotype and a state of enhanced inflammation.
Developing prevention strategies for Type 1 diabetes
For the first time, scientists were able to demonstrate that the lipid signaling generated by beta cells affects the body’s immune cells, resulting in inflammatory consequences. This suggests that lipids created by beta cells can cause their own death.
Continued research into this pathway may help scientists to develop effective prevention techniques to delay or even stop diabetes Type 1 establishing in an at-risk population.
Journal references:
Ashley, J., Hancock, W., Nelson, A., Bone, R., Tse, H., Wohltmann, M., Turk, J. and Ramanadham, S. (2016). Polarization of Macrophages toward M2 Phenotype Is Favored by Reduction in iPLA2β (Group VIA Phospholipase A2). Journal of Biological Chemistry, 291(44), pp.23268-23281. https://www.jbc.org/content/291/44/23268.short?utm_source=TrendMD&utm_medium=cpc&utm_campaign=Journal_of_Biological_Chemistry_TrendMD_0
Epstein, F., Atkinson, M., and Maclaren, N. (1994). The Pathogenesis of Insulin-Dependent Diabetes Mellitus. New England Journal of Medicine, 331(21), pp.1428-1436. https://www.ncbi.nlm.nih.gov/pubmed/7969282
Nelson, A., Stephenson, D., Cardona, C., Lei, X., Almutairi, A., White, T., Tusing, Y., Park, M., Barbour, S., Chalfant, C. and Ramanadham, S. (2019). Macrophage polarization is linked to Ca2+-independent phospholipase A2β-derived lipids and cross-cell signaling in mice. Journal of Lipid Research, 61(2), pp.143-158. https://pubmed.ncbi.nlm.nih.gov/31818877/