A new study published recently in eLife reports that researchers have developed new immunotherapy that eliminates solid tumors in mice without causing detrimental side effects.
This novel chimeric antigen receptor-T cell (CAR-T cell therapy) could be put to clinical trials very soon.
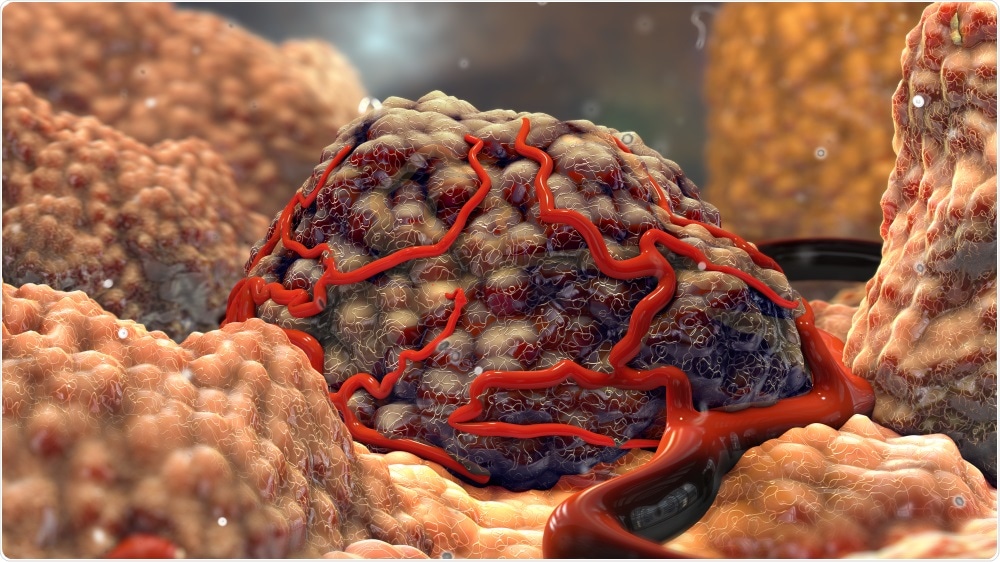
Image Credit: Nathan Devery/Shutterstock.com
Moreover, the researchers employed a new mouse model that can be used to verify the efficacy, safety, and mechanisms of CAR-T cell treatments for patients suffering from solid cancers, in the years to come.
CAR-T cell therapy involves collecting immune cells known as T cells from the blood samples of patients and reprogram the cells with CAR molecules that identify the cancer-specific antigens expressed on the cancer cells.
Upon administering CAR-T cells back to patients, they not just destroyed the antigen-expressing cancer cells directly but also turn on the immune system to fight against the tumor.
One of the challenges with developing CAR-T cells is that, sometimes, the CAR-T cells work against tumor antigens that are also present in lower amounts on normal cells, causing serious side effects which we only find out about in clinical trials.”
Tomonori Yaguchi, Study Co-Corresponding Author, Visiting Assistant Professor, Division of Cellular Signaling, Institute for Advanced Medical Research, Keio University School of Medicine
Yaguchi continued, “We proposed that if human CAR-T cells can cross-react with the mouse antigens and detect antigens found on normal mouse cells, we could test human CAR-T cells in mouse tumor models. This would allow more robust tests of both safety and effectiveness before the treatments reach clinical testing.”
The researchers formulated a CAR-T cell treatment that targets an antigen named glycipan-1 (GPC1), which can be found in huge amounts on various types of human cancer cells, and also in trace amounts on normal human and mouse cells. When the CAR-T cells were tested on mice carrying tumors, they discovered that the cells efficiently blocked tumor growth without any adverse reactions.
It was found that for one of the types of mouse tumors, four out of five of the mice that received CAR-T cell treatment remained completely tumor-free for at least 100 days. It was also found that the CAR-T cells improved immune responses against other tumor antigens compared to GPC1.
Drugs called immune checkpoint inhibitors are one of the most vital novel immunotherapy treatments for cancer. They act by activating blocked immune cells so that they can kill the cancerous cells.
The researchers combined the CAR-T cells with a checkpoint inhibitory drug that inhibits the activity of the PD1-protein in T cells and found that it increased the anti-tumor effects of CAR-T cell treatment. However, the checkpoint inhibitor alone had no effect individually. This shows that the use of CAR-T cells that target GPC1 together with a checkpoint inhibitor could be an effective combination for cancer treatment.
We have generated CAR-T cells targeting GPC1 in both humans and mice and shown their effectiveness in mouse solid tumor models. By establishing a new type of model, we were able to test the effectiveness, safety and anti-tumor mechanisms of CAR-T cells, showing the importance of choosing the most appropriate models for evaluating these novel types of cancer treatment.”
Yutaka Kawakami, Study Senior Author and Professor, Division of Cellular Signaling, Institute for Advanced Medical Research, Keio University School of Medicine
Source:
Journal reference:
Kato, D., et al. (2020) GPC1 specific CAR-T cells eradicate established solid tumor without adverse effects and synergize with anti-PD-1 Ab. eLife. doi.org/10.7554/eLife.49392.