Globally, researchers are racing against time to design a vaccine to guard against the COVID-19 infection, and epidemiologists are taking efforts to predict the way the coronavirus pandemic will spread until the availability of such a vaccine.
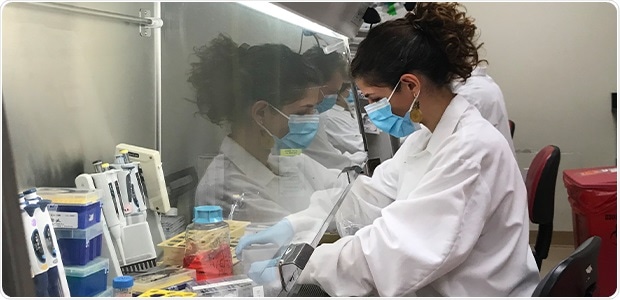
Alba Grifoni, PhD, an instructor in the Sette lab and the study’s co-first author, tests the T cell response in blood samples collected from individuals who have recovered from COVID-19. Image Credit: La Jolla Institute for Immunology.
However, both efforts are still shrouded by unresolved ambiguity as to whether the immune system can put up a significant and enduring response to the SARS-CoV-2 virus and whether any kind of protective immunity is provided by exposure to the circulating common cold coronaviruses.
An association between the laboratories of Alessandro Sette, Dr. Biol. Sci., and Shane Crotty, Ph.D., at La Jolla Institute for Immunology, is beginning to close the huge knowledge gap with excellent news for vaccine developers and is offering the first cellular immunological information to help guide recommendations for social distancing.
The study, published recently in the online edition of the Cell journal, records a powerful antiviral immune response to the SARS-CoV-2 virus in a cohort of 20 adults who had recovered from the COVID-19 infection.
These findings demonstrate that the immune system of the body is able to detect the SARS-CoV-2 virus in several ways, dismissing fears that the virus may evade ongoing efforts to develop an effective vaccine.
If we had seen only marginal immune responses, we would have been concerned, but what we see is a very robust T cell response against the spike protein, which is the target of most ongoing COVID-19 efforts, as well as other viral proteins. These findings are really good news for vaccine development.”
Alessandro Sette, Professor, Center for Infectious Disease and Vaccine Research, La Jolla Institute for Immunology
According to Crotty, “All efforts to predict the best vaccine candidates and fine-tune pandemic control measures hinge on understanding the immune response to the virus. People were really worried that COVID-19 doesn’t induce immunity, and reports about people getting re-infected reinforced these concerns, but knowing now that the average person makes a solid immune response should largely put those concerns to rest.”
Crotty is also a professor in the Center for Infectious Disease and Vaccine Research.
In previous research, Sette and his research team had employed bioinformatics tools to estimate which SARS-CoV-2 fragments have the potential to activate the human T cells.
In their latest study, the researchers tested whether the T cells, collected from adults who had recovered from the COVID-19 infection without any major problems, detected the so-called peptides, or the predicted protein fragments, from the virus itself.
The researchers combined the peptides under two huge groups. The first so-called mega-pool group contained peptides that cover all proteins in the viral genome, except for the “spike” protein of SARS-CoV-2. The second mega-pool especially targeted the spike protein that dots the surface of the virus, since nearly all vaccines being developed are currently targeting this spike protein of the coronavirus.
We specifically chose to study people who had a normal disease course and didn’t require hospitalization to provide a solid benchmark for what a normal immune response looks like, since the virus can do some very unusual things in some people.”
Alessandro Sette, Professor, Center for Infectious Disease and Vaccine Research, La Jolla Institute for Immunology
The scientists discovered that all the patients infected by COVID-19 had a solid CD4 or helper T cell response, which aids in the production of antibodies. Nearly all the patients had produced virus-specific killer, or CD8, T cells, which eliminate the cells infected by the virus.
Crotty stated, “Our data show that the virus induces what you would expect from a typical, successful antiviral response.”
Even though these outcomes do not disqualify that the immune response to the SARS-CoV-2 virus can be detrimental, they do offer a significant baseline against which immune responses of the individuals can be compared; or as Sette emphasized, “If you can get a picture of something, you can discuss whether you like it or not but if there’s no picture there’s nothing to discuss.”
We have a solid starting foundation to now ask whether there’s a difference in the type of immune response in people who have severe outcomes and require hospitalization versus people who can recover at home or are even asymptomatic.”
Alessandro Sette, Professor, Center for Infectious Disease and Vaccine Research, La Jolla Institute for Immunology
Sette continued, “But not only that, we now have an important tool to determine whether the immune response in people who have received an experimental vaccine resembles what you would expect to see in a protective immune response to COVID-19, as opposed to an insufficient or detrimental response.”
In addition, the researchers observed the response of T cells in blood samples that had been taken between 2015 and 2018, before the SARS-CoV-2 virus started to spread. A majority of these individuals have considerable T cell reactivity against SARS-CoV-2, even though they had never been exposed to this virus.
However, all of them have almost certainly witnessed at least three of the four common cold coronaviruses, which may explain the observed crossreactivity.
However, it is still not clear whether the observed crossreactivity offers at least a certain level of preexisting immunity to the SARS-CoV-2 virus and thus may explain why geographical locations or specific people are more severely affected by COVID-19.
“Given the severity of the ongoing COVID-19 pandemic, any degree of cross-reactive coronavirus immunity could have a very substantial impact on the overall course of the pandemic and is a key detail to consider for epidemiologists as they try to scope out how severely COVID-19 will affect communities in the coming months,” concluded Crotty.
Source:
Journal reference:
Grifoni, A., et al. (2020) Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. doi.org/10.1016/j.cell.2020.05.015.