Scientists have created a human cell “membrane on a chip” that enables continuous tracking of the interaction of drugs and infectious agents with the human cells. This membrane on a chip may soon be used for testing promising drug candidates for COVID-19.
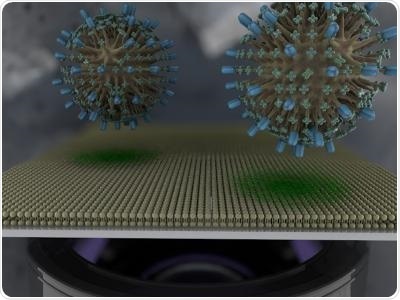
Researchers have developed a human cell ‘membrane on a chip’ that allows continuous monitoring of how drugs and infectious agents interact with our cells, and may soon be used to test potential drug candidates for COVID-19. Image Credit: Susan Daniel/Cornell University.
According to the research team from the University of Cambridge, Cornell University, and Stanford University, their novel device could imitate any type of cell, whether human, bacterial or even the hard cell walls of plants. The researchers’ study has recently focused on how COVID-19 attacks the cell membranes in humans, and more significantly, how it can be inhibited.
The devices have been developed on chips, making sure that the functionality and orientation of the cell membrane are intact. These devices have been effectively used for tracking the activity of ion channels—a group of proteins found in human cells and the target for over 60% of approved drugs. The study results have been published in two new articles in Langmuir and ACS Nano.
Cell membranes are known to play a vital role in biological signaling, regulating everything from pain relief to infections caused by a virus, serving as the gatekeeper between a cell and the exterior world.
The researchers set out to develop a sensor that maintains all the crucial aspects of a cell membrane, that is, fluidity, structure, and control across the movement of ions without the time-steps required to sustain a cell.
The device makes use of an electronic chip to quantify the variations in an overlying membrane derived from a cell, allowing the researchers to easily and safely interpret the interaction between the cell and the outside world.
The device incorporates cell membranes with conducting polymer electrodes as well as transistors. The research team from Cornell University developed the on-chip membranes by initially optimizing a procedure to create membranes from live cells and, subsequently, working with researchers from the University of Cambridge, coaxed them onto polymeric electrodes such that all their functionality was preserved.
The hydrated conducting polymers offer a more “natural” setting for the cell membranes and enable powerful tracking of the function of membranes.
The Stanford researchers improved the polymeric electrodes to track the modifications in the membranes. The new device no longer depends on live cells that are usually technically hard to keep them alive and require considerable attention, and quantifications can last across a long period of time.
Because the membranes are produced from human cells, it’s like having a biopsy of that cell’s surface - we have all the material that would be present including proteins and lipids, but none of the challenges of using live cells.”
Susan Daniel, Study Senior Author and Associate Professor, Department of Chemical and Biomolecular Engineering, Cornell University
According to Owens, “This type of screening is typically done by the pharmaceutical industry with live cells, but our device provides an easier alternative. This method is compatible with high-throughput screening and would reduce the number of false positives making it through into the R&D pipeline.”
The study was published in the ACS Nano journal.
The device can be as small as the size of a human cell and easily fabricated in arrays, which allows us to perform multiple measurements at the same time.”
Anna-Maria Pappa, University of Cambridge
Pappa is also the joint first author on both papers.
So far, the goal of the study, assisted by funding from the United States Defense Research Projects Agency (DARPA), was conducted to show how viruses like influenza communicate with cells. DARPA has now offered more funding to examine the effectiveness of the device in screening for promising drug candidates for COVID-19 in a safe and efficient manner.
Considering the substantial risks to scientists focused on SARS-CoV-2, the virus that is responsible for causing COVID-19, researchers working on the project will work on making virus membranes and merging those with the chips.
Identical to the SARS-CoV-2 membrane, the virus membranes lack the viral nucleic acid. In this manner, novel antibodies or drugs to neutralize the virus spikes that are employed to penetrate the host cell can be detected. The study is anticipated to start on August 1st, 2020.
With this device, we are not exposed to risky working environments for combating SARS-CoV-2. The device will speed up the screening of drug candidates and provide answers to questions about how this virus works.”
Han-Yuan Liu, Study Joint First Author and Researcher, Cornell University
Upcoming studies will work on improving the production of the devices at Stanford University and automating the fusion of membranes with the chips, exploiting the fluidics know-how from Stanford PI Juan Santiago who will join the research team in August 2020.
“This project has merged ideas and concepts from laboratories in the UK, California and New York, and shown a device that works reproducibly in all three sites. It is a great example of the power of integrating biology and materials science in addressing global problems,” Alberto Salleo, Stanford lead PI Professor, concluded.
Source:
Journal reference:
Liu, H.-Y., et al. (2020) Self-Assembly of Mammalian-Cell Membranes on Bioelectronic Devices with Functional Transmembrane Proteins. ACS Langmuir. doi.org/10.1021/acs.langmuir.0c00804.