Researchers from the Albert Einstein College of Medicine have demonstrated that chronic psychological stress can result in painful vessel-clogging episodes—a frequent cause of hospitalizations and the most typical complication of sickle-cell disease or SCD.
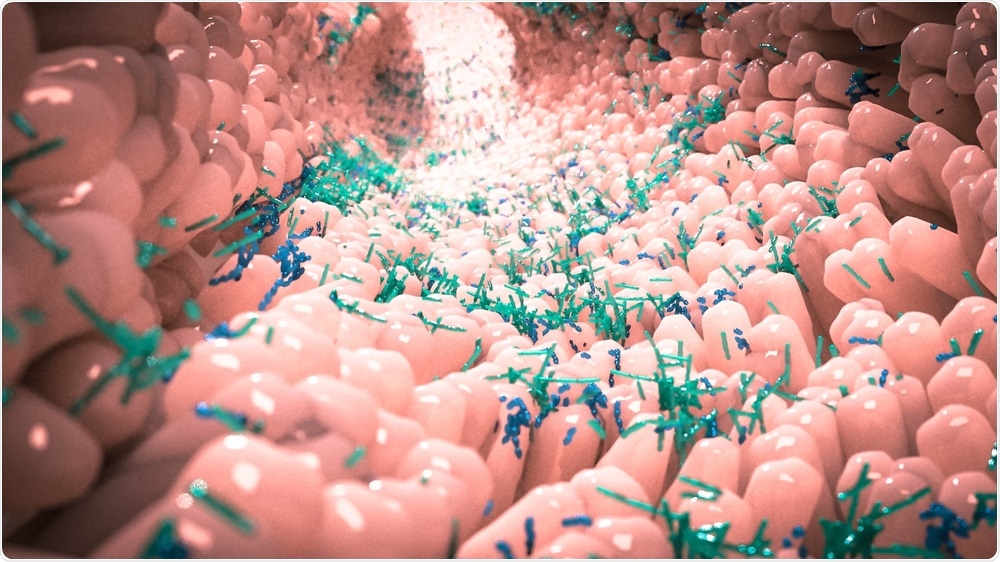
Image Credit: Alpha Tauri 3D Graphics/Shutterstock.com
This discovery was made in mice and demonstrated that the gut microbiome has a crucial role to play in activating those painful episodes and shows potential approaches to prevent them.
The study was recently published online in the Immunity journal.
One in 365 African-American births has SCD. Individuals suffering from SCD inherit a genetic mutation that results in atypical hemoglobin, causing hemoglobin-containing red cells to assume a sickle shape and thus become less flexible.
These sickled red cells clog tiny vessels, and as a result, blood flow is obstructed and oxygen is prevented from reaching the tissues. This can lead to debilitating and painful vaso-occlusive episodes (VOEs), which can continue for days.
VOEs could not be reversed by any treatment and, over time, they cause considerable damage to the internal organs. This is the reason why individuals suffering from severe SCD have a shorter life expectancy of 20 to 30 years when compared to those without this disorder.
Research for sickle-cell disease is chronically underfunded and those with the condition are in need—and deserve—new treatments that can help address this major health disparity. We hope our most recent findings can help point to novel solutions for treating this painful and deadly disease.”
Paul S. Frenette, MD, Study Lead and Professor, Departments of Medicine and Cell Biology, Albert Einstein College of Medicine
Dr Frenette is also the chair and director of the Ruth L. and David S. Gottesman Institute for Stem Cell and Regenerative Medicine Research at the same college.
With the help of a mouse model, Dr Frenette and his collaborators discovered that the route to VOE starts in the brain. During stress, glucocorticoid hormones are secreted in the brain and find their way to the gut and boost its permeability.
A greater permeability like this enables segmented filamentous bacteria (SFB)—a kind of beneficial gut bacteria present in mice—to communicate with Th17 helper immune cells in the gut lining.
Those immune cells are activated by the SFB to release pro-inflammatory molecules, which, in turn, enter the circulation and support the accumulation and aging of neutrophils—a form of white blood cell. In a previous research work, the Frenette laboratory had discovered that such aged neutrophils are cells that induce inflammation and fuel the VOE.
This series of events was seen in both healthy mice and SCD mice that were exposed to psychological stress. But only mice with sickle-cell disease experienced the lethal VOE.
Healthy mice don’t have sickled blood cells and therefore don't suffer the ill effects caused by the buildup of aged neutrophils. Importantly, we found we could markedly reduce stress-induced VOE in mice through several different interventions: inhibiting the synthesis of glucocorticoids, depleting SFB, or blocking the inflammatory molecules induced by these bacteria.”
Paul S. Frenette, MD, Study Lead and Professor, Departments of Medicine and Cell Biology, Albert Einstein College of Medicine
Dr Frenette continued, “Each of those actions could potentially limit the impact of psychological stress on people with SCD.”
Although SFBs are present only in rodents, certain proof indicates that Th17 immune cells can also be induced by analogous beneficial bacteria present in the human gut to create inflammatory molecules.
“We hope to learn whether there is any correlation between the abundance of these bacteria in patients with sickle-cell disease and the frequency or severity of VOEs that affect them,” concluded Dr Frenette.
Source:
Journal reference:
Xu, C., et al. (2020) The Gut Microbiome Regulates Psychological-Stress-Induced Inflammation. Immunity. doi.org/10.1016/j.immuni.2020.06.025.