Researchers from Salk Institute have made a significant advancement in the quest for a safe, effective treatment for type 1 diabetes—a medical disorder that affects around 1.6 million Americans and costs $14.4 billion every year.
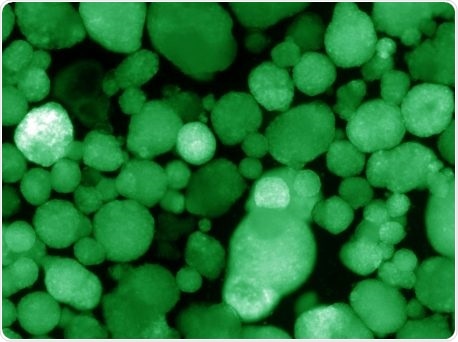
Human islet-like organoids express insulin, which is indicated by the green color. Image Credit: Salk Institute.
The Salk Institute team used stem cell technology and successfully produced the first human insulin-producing pancreatic cell clusters. These cells can escape the immune system, as described in the Nature journal on August 19th, 2020.
When these clusters of “immune shielded” cells were transplanted in the body of the mice, they regulated blood glucose even in the absence of immunosuppressive drugs in these animals.
Most type 1 diabetics are children and teenagers. This is a disease that is historically hard to manage with drugs. We hope that regenerative medicine in combination with immune shielding can make a real difference in the field by replacing damaged cells with lab-generated human islet-like cell clusters that produce normal amounts of insulin on demand.”
Ronald Evans, Study Senior Author and Professor, Salk Institute
Evans also holds the March of Dimes Chair in Molecular and Developmental Biology.
Type 1 diabetes is a permanent medical disorder that is still difficult to manage, even with the use of automated devices that supply insulin to control blood sugar levels.
Although transplants of pancreatic beta islets—groups of cells that make various hormones, including insulin—from donor tissues can treat this disorder, patients have to take immunosuppressing medications throughout their life, which pose a serious risk. For many years, scientists have sought a better method to restore the lost pancreatic cells.
Now, the device-free transplantation of insulin-producing cells brings scientists one step forward in treating the disease, stated the laboratory.
In an earlier study, the Evans laboratory resolved a barrier in the field, wherein stem-cell-derived beta-like cells created insulin, but were not working.
According to Evans, the cells did not discharge insulin in response to glucose, because they were simply under-powered. Evans’ research team eventually identified a genetic switch, known as ERR-gamma, that “turbo-charges” the cells upon flipping.
When we add ERR-gamma, the cells have the energy they need to do their job. These cells are healthy and robust and can deliver insulin when they sense high glucose levels.”
Michael Downes, Study Co-Author and Senior Staff Scientist, Salk Institute
A significant part of the latest research was to create a method to culture beta-like cells in a 3D setting that approximates the human pancreas. This provided an islet-like property to the cells. Most significantly, the researchers observed that a protein known as WNT4 can switch on the ERR-gamma-driven maturation switch.
This integration of steps created functional cell clusters that imitate human islets—the supposed human islet-like organoids (HILOs).
The team then addressed the complex problem of immune rejection. Standard tissue transplants need lifetime immune-suppressive treatments to guard the tissues against being attacked by the immune system. But these treatments also raise the risk of infections.
Motivated by the successes of immunotherapy medications designed for cancer, the researchers initially demonstrated that the transplanted cells were protected by the checkpoint protein PD-L1.
“By expressing PD-L1, which acts as an immune blocker, the transplanted organoids are able to hide from the immune system,” stated Eiji Yoshihara, the study’s first author and a former staff scientist in the laboratory.
Using short pulses of the protein interferon gamma, Yoshihara subsequently created a technique to induce the PD-L1 protein in HILOs.
When these immune-evasive HILOs were transplanted into diabetic mice, they offered sustained blood glucose control in diabetic mice that have healthy immune systems.
This is the first study to show that you can protect HILOs from the immune system without genetic manipulation. If we are able to develop this as a therapy, patients will not need to take immune-suppressing drugs.”
Michael Downes, Study Co-Author and Senior Staff Scientist, Salk Institute
More studies are required before this system can be progressed to clinical trials. The transplanted organoids should be tested in mice for extended periods of time to verify whether their impacts are long-lasting. In addition, more research needs to be performed to ensure that these organoids are safe enough to be used in human beings as well.
“We now have a product that could potentially be used in patients without requiring any kind of device,” Evans concluded.
First immune-evading cells created to treat type 1 diabetes
First immune-evading cells created to treat type 1 diabetes. Video Credit: Salk Institute.
Source:
Journal reference:
Yoshihara, E., et al. (2020) Immune-evasive human islet-like organoids ameliorate diabetes. Nature. doi.org/ 10.1038/s41586-020-2631-z.