Scientists have detected a second path to treat chronic myelogenous leukemia, which is known to affect older adults, despite the resistance to present-day drugs.
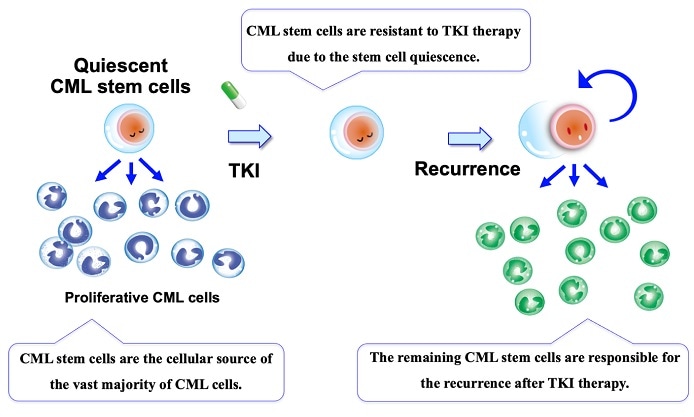
CML stem cells, which are the cellular source of the vast majority of CML cells, are reportedly resistant to TKI therapy due to the stem cell quiescence. Thus, the remaining CML stem cells are responsible for the recurrence after TKI therapy. Image Credit: Kazuhito Naka, Hiroshima University.
The latest findings were published in the Nature Communications journal on September 17th, 2020.
Nearly all patients suffering from chronic myelogenous leukemia (CML) have a defective cancer-causing gene, or “oncogene” known as BCR-ABL1. BCR-ABL1 converts a regular stem cell (a special type of cell that can change into other cell types and subsequently reproduce those cells during life time) in the bone marrow into a CML stem cell that creates malformed blood cells.
But the CML stem cell does not die as it was scheduled to do so, and rather the oncogene allows it to continue to produce even more of these defective blood cells.
Since the turn of the millennium, advancements in treatment have been highly successful at fighting the disease in patients who have this oncogene. Drugs known as tyrosine kinase inhibitors (TKI) have fully changed the prognosis of patients suffering from such leukemias, and with fewer of the side effects of other cancer therapies. In a majority of the cases, the cancer goes into remission and patients survive for several years even after diagnosis.
BCR-ABL1 controls the production of an unusual type of tyrosine kinase—an enzyme that “turns on” several types of proteins via a cascade of chemical reactions called signal transduction—in effect, communication through chemistry.
Miscommunicati emerging from the faulty enzyme is what supports the growth of the leukemic cells. TKI signal transduction therapy stops this interaction within the CML stem cells and suppresses their growth, eventually stopping their production of the malformed blood cells.
But TKIs only regulate the disease and do not treat it. A patient can develop drug resistance because while TKIs function well on proliferative mature CML cells that are intensively reproducing, they are not highly effective at promoting cell death on the part of quiescent CML stem cells.
Quiescence refers to an “idling” phase in the life cycle of a cell, wherein it primarily just rests and hangs out for prolonged periods of time in anticipation of reactivation—that is, neither dying nor replicating.
If CML stem cells are in a quiescent phase, they are otherwise left untouched by TKI treatment, and so survive to potentially cause a relapse.”
Kazuhito Naka, Study Author and Associate Professor, Department of Stem Cell Biology, Research Institute for Radiation Biology and Medicine, Hiroshima University
However, in mouse models, the team discovered that if they interrupt Gdpd3—a different, non-oncogene gene—the self-renewal potential of the CML stem cells is acutely reduced. The Gdpd3 gene guides the production of an enzyme for a specific type of lipid that seems to play a major role in controlling the quiescence of CML stem cells in an oncogene-independent manner.
To put this in simpler terms, the Gdpd3 gene involved in the producing this lipid is mostly responsible for maintaining the CML stem cells. The team had now broken their quiescence.
Most importantly, when the team disturbed the Gdpd3 gene encoding these lipids, leukemia relapse in the mice was considerably decreased, without the disruption of the BCR-ABL1 oncogene.
This potentially provides another path to arresting these leukemias—and maybe other cancers too, beyond having to wrestle with the BCR-ABL1 oncogene.”
Kazuhito Naka, Study Author and Associate Professor, Department of Stem Cell Biology, Research Institute for Radiation Biology and Medicine, Hiroshima University
Although the team has found a new, biologically important role for this specific lipid that is responsible for causing the recurrence of CML, they are still unable to interpret clearly how exactly this takes place.
Now, the researchers want to study the mechanisms involved and whether this kind of lipid also plays a key role in the quiescence of the cancer stem cells that are responsible for causing solid tumors, not only in leukemias but also in the growth and recurrence of cancers.
Source:
Journal reference:
Naka, K., et al. (2020) The lysophospholipase D enzyme Gdpd3 is required to maintain chronic myelogenous leukaemia stem cells. Nature Communications. doi.org/10.1038/s41467-020-18491-9.