After infection of the human body with a pathogen, a cascade of reactions will usually be set into motion. Amongst others, specific cells of the immune system known as T cells get activated in the lymph node and will subsequently divide and proliferate.
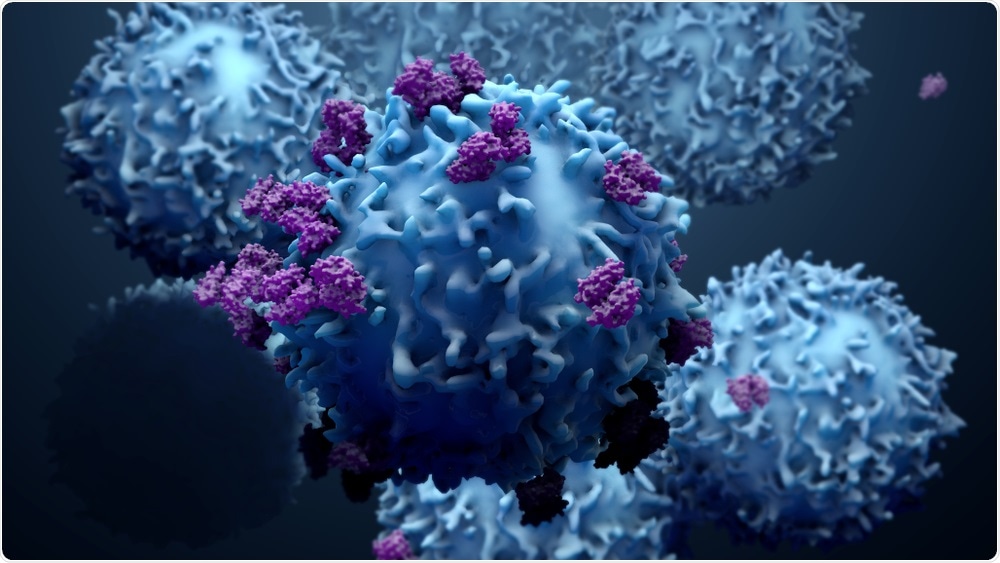
Image Credit: Design_Cells/Shutterstock.com
At the same time, these cells will gain certain functions, that enable them to destroy other cells, that are e.g. infected by a virus. In addition, they produce certain proteins - so-called cytokines - with which they can stop the reproduction of the pathogen.
The immune system and its function are the main focus of the research of Professor Wolfgang Kastenmueller, director of the Chair of Systems Immunology I at the Institute of Systems Immunology of the Julius-Maximiliams-Universität Würzburg (JMU). Together with Professor Georg Gasteiger, director of the Chair of Systems Immunology II, they lead the Max-Planck Research group of Systems Immunology.
Their research focus is the interaction of the immune system with the organism, especially the interaction of different cells of the immune system within local networks and with other cells of other organ systems.
Publication in Nature Immunology
Recently Kastenmueller and his team deciphered new details of the functioning of the immune system, which are important for the immune system to remember recent infections. Their results have been published in the latest issue of the scientific journal Nature Immunology. Their findings could help to improve immune therapy towards tumor diseases.
"If a body has fought and eliminated a pathogen successfully, most of the recently proliferated T cells are no longer needed and will die", Wolfgang Kastenmueller explains. But about five to ten percent of these cells survive and develop into a long lasting "memory population", that will protect the body against future infections.
Improvement of the immunological memory
Kastenmueller describes the main result of his study : "In our recent work we identified a transcription factor - BATF3, that very specifically regulates the survival of these cells and therefore the transition into a memory response". The scientists could show that this factor only gets produced shortly after the initial activation of T cells. The absence of this factor leads to a permanent malfunction of the memory response.
Until now the role of this factor for so-called CD8+ T cells was unclear. It was only after the scientists overexpressed this factor in CD8+ T cells that the importance became clear, as they could see that the survival of these cells and thus the immunological memory improved significantly.
This study was conducted in close collaboration with the Medical Clinic II of the University clinic of Wuerzburg. It combines basic research with applied medicine and could help to develop better therapies for cancer treatments that use the immune system of the patient - so-called CAR-T cell therapy.
Using CAR-T cell therapy, T cells get extracted from the blood of the patient and are subsequently genetically modified with the chimeric antigen receptor (CAR) molecules. This modification enables T cells to attack tumor cells, which they couldn't biochemically detect before. These modified T cells are subsequently transferred back into the patient.
Currently CAR-T cells are successfully used for therapies for diseases such as B cell lymphoma, a malignant disease of the lymphatic system. Kastenmueller and his team together with Professor Michael Hudecek of the Medical Clinic II are now planning to modify CAR-T cells so as to improve the survival of the patients and thus the therapeutic efficiency.