Ligament injuries that affect scores of regular citizens and athletes are sidelined every year. Added to this, recovery is painful and takes a long time and, at times, a return to normal function is never achieved because of the formation of scars—an aspect that makes ligament injuries inclined to more damage.
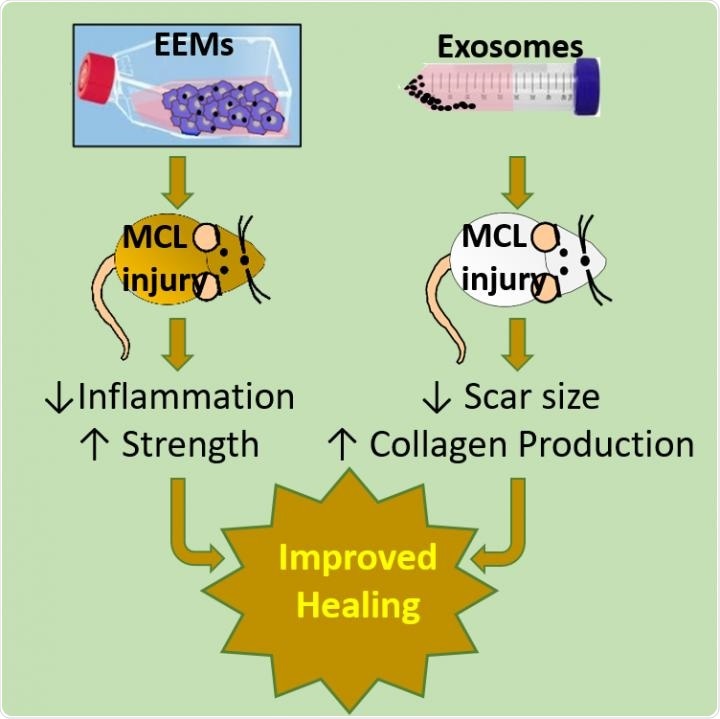
Exosome educated macrophages (EEMs) and exosomes differentially improve ligament healing. EEM treatment to an injured rat medial collateral ligament (MCL) resulted in reduced inflammation and improved ligament strength. In contrast, exosome treatment reduced scar size and increased collagen organization and production. Despite different outcomes, both treatments were uniquely effective in accelerating healing. Image Credit: AlphaMed Press.
A novel exosomes study, which was recently published in the STEM CELLS journal, may offer a suitable solution in the days to come.
Exosomes are sacs of cell membranes found in the body which transport genetic and protein information between cells, and similarly, exosome-educated macrophages (EEMs) are a form of white blood cell that generally destroys microbes and eliminates dead cells, but could also trigger the action of other immune system cells. The research shows how these exosomes and EEMs can reduce scarring and promote the healing of ligaments.
In 2019, the researchers behind this study, that is, scientists from the University of Wisconsin-Madison (UW-Madison), reported another study, which was also published in the STEM CELLS journal. This study demonstrated that treating an Achilles tendon with EEMs not only decreased the inflammation but also improved the strength of the tendon.
The EEMs were produced by subjecting the CD14+ macrophages to mesenchymal stromal cell (MSC)-derived exosomes.
Our previous study was done on a mouse model. While the results were superior when compared to treatment with MSCs, the functional/mechanical benefit of the exosomes was not as obvious as with the EEMs. This led us to our current study goals.”
Ray Vanderby, PhD, Professor of Orthopedics and Rehabilitation, University of Wisconsin-Madison
Vanderby and Peiman Hematti, MD, from the Department of Medicine at the University of Wisconsin-Madison are the corresponding authors of the two studies.
Firstly, the team wanted to recreate the healing effects of EEMs in a different model of rodent—that is, a rat medial collateral ligament (MCL); this ligament runs along the knee’s edge.
Dr. Vanderby added, “We hypothesized the EEM treatment would reduce inflammation and accelerate ligament healing, similar to our previous tendon results.”
Secondly, the team wanted to examine the effects of exosome treatment on the MCL injuries of rats, speculating that MSC-derived exosomes could also decrease the formation of scars and enhance ligament healing.
Once the results came in, they supported the researchers’ speculation that EEMs indeed enhanced the MCL function of rats and also decreased the ratio of M1/M2 macrophages (while M1 macrophages guard against viruses and bacteria, M2 macrophages target tissue repair and wound healing.). In addition, the exosomes triggered a biological response—most significantly, a reduction in scarring and an increase in collagen.
Dr. Vanderby added, “The ability of exosomes to reduce scar formation and upregulate collagen type expression has been documented in tendon healing models, but to our knowledge, this is the first study to report this in ligaments.”
This study is an exciting advance in the field of MSC-derived exosomes, the demonstration by this excellent group that exosome-educated macrophages can play such a major role in both tendon and ligament healing has exciting potential for improving the trajectory of healing of human athletic injuries.”
Dr Jan Nolta, Editor-in-Chief, STEM CELLS
Now, the researchers’ question is whether, apart from supporting the healing of tendon- and ligament- related injuries, exosomes, and EEMs may also be used on other scarring debilities.
Of major interest to the team is how the exosomes and EEMs might be used for treating a broad range of sport-related orthopedic and degenerative conditions. But exosome and EEMs could also be studied in a broad range of other applications, like radiation damage caused to the bone marrow. For Dr Hematti, who is a bone marrow transplant physician, radiation damage to the bone marrow is another field of special interest.
EEMs and exosomes each have attractive characteristics as therapeutics. As a cell therapy, EEMs will not proliferate or differentiate to undesirable cell types, which remains a concern for many stem cell therapies. Moreover, EEMs could be generated from a patient’s own monocytes using off-the-shelf exosomes, resulting in a faster and more facile process compared to autologous MSCs. Alternatively, exosome therapy could be a cell-free, shelf-stable therapeutic to deliver biologically active components.”
Peiman Hematti, MD, Study Corresponding Author, Department of Medicine, University of Wisconsin-Madison
“Altogether, we believe our studies’ results support the use of EEMs and/or exosomes to improve ligament healing by modulating inflammation and tissue remodeling,” concluded Dr Vanderby.