In COVID-19 patients with severe lung disease, targeting the endothelial cells—that is, cells comprising the blood vessel wall, which control oxygen exchange between the bloodstream and airways—may be an innovative strategy to restore normal function of the lungs.
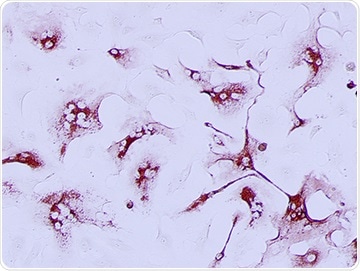
SARS-CoV-2 infection in endothelial cells. Image Credit: Stony Brook University.
This theory emerges from a study performed by scientists in the Department of Microbiology and Immunology in the Renaissance School of Medicine at Stony Brook University and reported in mBio, the prominent journal of the American Society for Microbiology.
SARS-CoV-2, which is responsible for causing COVID-19, is distinguished by viral pneumonia, pulmonary edema, inflammation, coagulopathy, and other physiological abnormalities. Angiotensin-converting enzyme 2 (ACE2) receptors are used by SARS-CoV-2 to infect and impair the ciliated epithelial vascular cells in the upper respiratory tract.
But the mechanism used by the SARS-CoV-2 virus to dysregulate the vascular functions that cause an acute respiratory distress syndrome (ARDS) in COVID-19 patients continues to be elusive.
The research team, headed by Erich Mackow, PhD, a Professor of Microbiology and Immunology, set out to explore this mechanism by analyzing SARS-CoV-2 infection of human endothelial cells in the brain, lungs, heart, and kidneys that are affected in COVID-19 patients.
Claims that endothelial cells are infected by SARS-CoV-2 through ACE2 receptors have never been assessed directly. Our research revealed that endothelial cells lack ACE2 receptors and that endothelial cells were only SARS-CoV-2 infected after expressing ACE2 receptors in them. Since endothelial cell functions are dysregualated by SARS-CoV-2, these findings suggest a novel mechanism of regulation that does not require viral infection.”
Erich Mackow, PhD, Professor of Microbiology and Immunology, Stony Brook University
Professor Mackow continued, “Instead it suggests the indirect activation of the endothelium, potentially resulting from surrounding tissue damage that could be the basis for further research to therapeutically target and restore normal endothelial cell responses.”
Professor Mackow added that their study focuses on both ACE2 functions and endothelial cells in COVID-19 disease to identify mechanisms of capillary inflammation and abnormal clotting inside the vessels. He described that the study shows a new mechanism for clotting and endothelial inflammation seen in the heart and lungs of COVID-19 patients.
“A transformative change in the mechanism of endothelial cell dysfunction, not the infection of the cells themselves, changes the way in which disease is initiated and rationales for therapeutic targeting. If endothelial cells are not infected or directly damaged, they can still direct inflammation and clotting by just being activated,” Professor Mackow concluded from the study outcomes.
The researchers are working on how endothelial cells can be stimulated by the virus or in reaction to other SARS-CoV-2-infected lung cells expressing ACE2 receptors.
Instead of endothelium infection, the study indicates the possibility to therapeutically target activation as a new approach for resolving coagulation and inflammatory symptoms of COVID-19.
Mackow highlighted that more studies of endothelial cells, as well as down-regulated ACE2 functions after SARS-CoV-2 infection, are required to establish targets that could result in reduced respiratory distress and symptoms of COVID-19 patients.
Source:
Journal reference:
Conde, J. N., et al. (2020) Recombinant ACE2 Expression Is Required for SARS-CoV-2 To Infect Primary Human Endothelial Cells and Induce Inflammatory and Procoagulative Responses. mBio. doi.org/10.1128/mBio.03185-20.