According to a research team headed by the University of Connecticut Health, a sugar-binding protein could drive terrible inflammation and worsen sepsis—a disease that kills over 270,000 individuals per year in the United States alone. The study was published in the January 4, 2021 issue of the Nature Immunology journal.
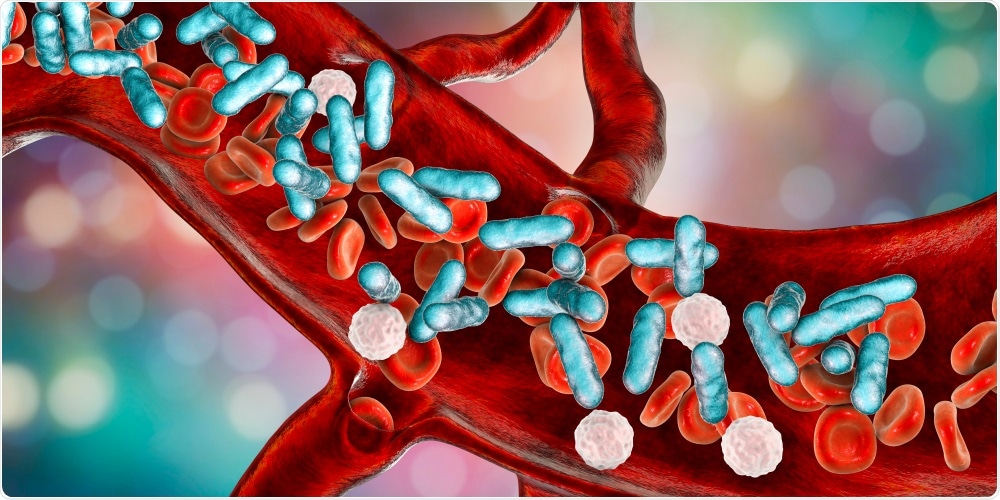
Sepsis. Image Credit: Kateryna Kon/Shutterstock.com
Sepsis is mainly caused by bacterial infections. The immune system becomes uncontrollable and activates a cytokine storm—a condition in which proteins that cause inflammation enter the blood. Organs may break down, and this is often followed by death.
Cytokine storms can also be caused by other diseases; according to medical researchers, cytokine storms account for the lethality of the 1918-1919 flu epidemics, and also the Black Death. Moreover, cytokine storms are seen in patients with severe COVID-19 infection and considered to play a role in COVID-19-related deaths.
The main cause for the cytokine storms during sepsis is the excessive reaction of the body when it recognizes an infection within the cells. When a cell identifies bacteria or bacterial pieces within itself, it directly stimulates enzymes that consequently trigger a protein that makes holes on the cell membrane from within, ultimately causing the cell to explode and release cytokines into the bloodstream. Cytokines are warning signals, calling in the immune system to combat the bacteria.
In addition, cytokines could cause other cells to explode and sound the alarm. The system normally damps itself and settles down after a while; however, in sepsis, it runs out of control, causing an increasing number of cells to burst and die and discharge even more cytokines into the bloodstream.
Whenever cells break open, they discharge cytokines and also other dangerous molecules, known as alarmins, that warn the body about an injury or infection and can increase the ongoing cytokine storm.
Vijay Rathinam, an immunologist from the University of Connecticut Health, wanted to find out which alarmins were discharged when a cell identified a particular kind of bacterial molecule known as lipopolysaccharide within itself.
Dr Ashley Russo, who was a graduate student in the Rathinam laboratory, cataloged—in association with immunologists Tony Vella and Antoine Menoret from the University of Connecticut Health—proteins discharged by these cells when they identified lipopolysaccharide.
The researchers discovered an amazing thing—a protein called Galectin-1 that binds sugars and sugar-coated proteins, appeared to be emanating from the cells. Fascinatingly, the team discovered that the galectin-1 is sufficiently small to slip out of the holes poked in the membrane of the cells, right before the cells explode.
When the researchers observed that, they started to study the role galectin-1 played in sepsis. They noted that galectin-1 appeared to be blocking a brake on inflammation, causing the cytokine storm to build up.
Moreover, they discovered that mice lacking the galectin-1 protein had less organ damage, less inflammation, and lived longer than standard mice did during sepsis, leading to a bacterial infection and lipopolysaccharide.
The researchers teamed up with Drs Deshmukh, Bauer, and Sponholz from the Jena University Hospital to find out if galectin-1 is discharged during sepsis in human patients, and observed that sepsis patients had greater levels of galectin-1 when compared to healthy people and other non-sepsis patients in emergency care.
The researchers are considering whether the galectin-1 protein might be an excellent drug target to help reduce cytokine storms during sepsis and also a handy marker that could be used by doctors to identify critical ill patients at risk.
Source:
Journal reference:
Russo, A. J., et al. (2021) Intracellular immune sensing promotes inflammation via gasdermin D–driven release of a lectin alarmin. Nature Immunology. doi.org/10.1038/s41590-020-00844-7