Chimeric Antigen Receptor T-cell therapy (CAR T) has transformed the treatment for leukemia. Regrettably, the therapy is not effective enough to treat solid tumors, including childhood cancers like neuroblastoma. Preclinical studies that used specific CAR T against neuroblastoma showed toxic effects.
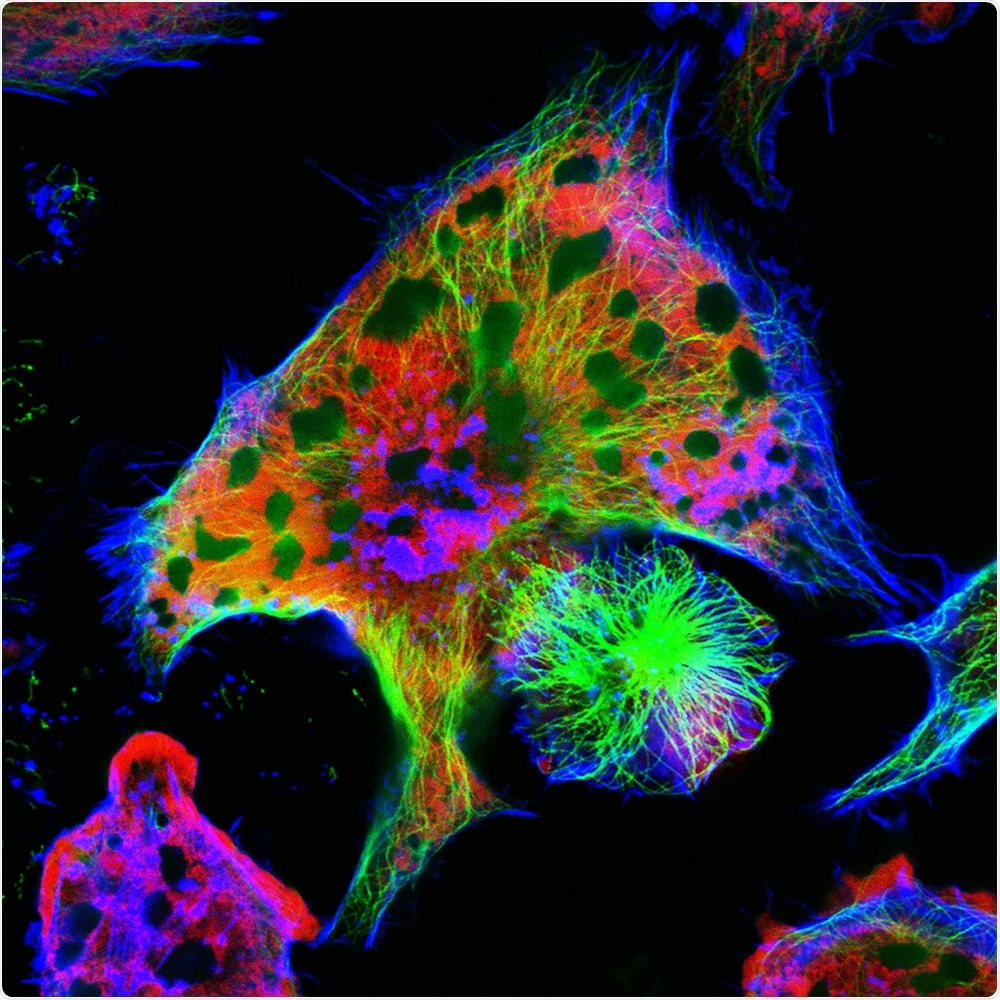
Image Credit: Vshivkova/Shutterstock.com
A research team from Children’s Hospital Los Angeles has now created an altered version of CAR T that shows potential in targeting neuroblastoma, destroys the cancer cells more effectively, and spares healthy brain tissue.
The study was recently published in the Nature Communications journal. While the study is still in the preclinical phase, it shows potential for lifesaving treatment in adults and children with solid tumors.
Shahab Asgharzadeh, MD, a physician-scientist from the Cancer and Blood Disease Institute of CHLA, is working to enhance the lifesaving CAR T-cell therapy, in which the team extracts the T-cells from the patient’s own immune system and engineer them to identify and kill cancer cells.
The CAR T therapy works in leukemia, by targeting a unique protein (or antigen) on the surface of leukemia cells. When the treatment is given, leukemia cells are killed. CAR T turns the patient's immune system into a powerful and targeted cancer-killer in patients with leukemia. This antigen is also on normal B cells in the blood, but this side effect can be treated medically.”
Dr Shahab Asgharzadeh, MD, Physician Scientist, Cancer and Blood Disease Institute, Children’s Hospital Los Angeles
Conversely, solid tumors such as neuroblastoma or breast cancer present a dilemma. The majority of the antigens found on their surface are also present in healthy tissues, in which toxicity cannot be controlled safely, as in the case of leukemia. In patients suffering from a solid tumor, CAR T cell therapy destroys both cancer cells and healthy tissues extensively.
Due to this reason and the suppressive immune environment inside the solid tumor, preclinical studies targeting these cancers resulted in only minimal efficacy or intolerable toxicity levels.
CAR T therapy is incredibly powerful, but for solid tumors it has significant barriers. We needed a way to boost the CAR T-cells to make them fight harder and smarter against the cancer. But we also want to save brain cells and other healthy tissue.”
Babak Moghimi, MD, Study First Author, Children’s Hospital Los Angeles
And this is precisely what the team did.
The researchers employed a novel CAR T technology, known as synthetic Notch (or synNotch). SynNotch CAR T-cells have a special property—referred to as gating—that enables them to target particular cancers very accurately. The gating function operates just like logic gates—a tool generally employed by computer programmers: if condition A is met, then do actions B.
According to Dr. Moghimi, “The way it works is really unique.” He described that the unique synNotch protein found on the T-cell surface is engineered to detect the GD2 antigen. When it does, the synNotch protein sends an instruction to the T-cell to stimulate its CAR T properties, allowing its potential to identify a second antigen, called B7H3. The T-cell needs to follow these particular instructions, which implies that it can only destroy cells with both antigens.
This gating trait is the main factor to reduce toxicity; at times, healthy cells will have low concentrations of one of the antigens, but not both. Solid tumors, such as neuroblastoma, have both B7H3 and GD2 antigens, which Dr. Asgharzadeh group has engineered the synNotch cells to identify.
The researchers were also able to overcome another challenge.
With normal CAR T therapy, the CAR T-cells burn out and are no longer active after some time. But we discovered the synNotch CAR T-cells are more metabolically stable because they are not activated constantly.”
Dr Shahab Asgharzadeh, MD, Physician Scientist, Cancer and Blood Disease Institute, Children's Hospital Los Angeles
This implies that the CAR T-cells use minimal energy, which enables them to continue to combat cancer for a longer period of time.
Source:
Journal reference:
Moghimi. B., et al. (2021) Preclinical assessment of the efficacy and specificity of GD2-B7H3 SynNotch CAR-T in metastatic neuroblastoma. Nature Communications. doi.org/10.1038/s41467-020-20785-x.