A few patients suffering from melanoma are known to respond quite well to immunotherapy and experience significant and long-lasting tumor regression.
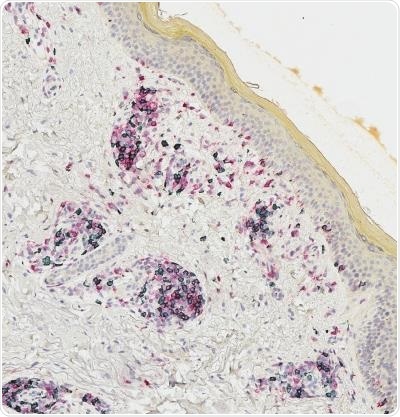
Microscopic image of patient vitiligo-affected skin containing resident memory T cells (outlined in black). Image Credit: Shaofeng Yan.
A subset of these patients will also acquire autoimmunity against their normal melanocytes—the cells that lead to melanoma—a phenomenon known as vitiligo.
For many years, melanoma survivors affected by vitiligo have been recognized as a unique group that has an excellent prognosis and a robust response of immune system cells, known as T cells.
Immunotherapy scientists from Dartmouth-Hitchcock’s Norris Cotton Cancer Center (NCCC), headed by Mary Jo Turk, Ph.D. and surgical oncologist Christina Angeles, MD (currently at the University of Michigan), have found how a subset of T cells called memory T cells are produced in melanoma survivors affected by vitiligo and able to work for years after tumor regression.
We are trying to understand how immune responses against cancer can persist over long periods of time in patients who have excellent responses to immunotherapy. Our study was aimed at discovering where T cells go, what they do and how long they last in these patients. Some T cells last a short time, but others, known as memory T cells, can last for years. The goal of this work was to understand how memory T cells are generated in these patients.”
Mary Jo Turk, PhD, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center
During the study, Turk and Angeles found that T cells entering melanoma tumors also tend to penetrate the vitiligo-affected skin of the patient; this skin builds up a more focused collection of tumor-associated T cells when compared to blood; and that T cells present in melanoma tumors are molecularly and genetically quite analogous to those in vitiligo-affected skin.
Based on these results, the researchers subsequently detected a new subset of “resident memory” (TRM) cells that localize to a patient’s tumor and skin and create high concentrations of the cytokine interferon-gamma.
TRM-IFNγ cells feature a special “signature,” or gene expression profile, found in melanoma tumors of patients who have lived longer than those who lack the signature. Both Turk and Angeles discovered that T cells infiltrating the tumors have corresponding daughter cells, or clonal partners, that remain in the skin and blood of the patient for up to nine years later.
The study titled “Resident and circulating memory T cells persist for years in melanoma patients with durable responses to immunotherapy,” has been recently published in the Nature Cancer journal.
No previous studies have shown cellular proof of such long-lived immunity to tumors. In the extensive association between surgeons, researchers, and oncologists tumors, skin, and blood were harvested from melanoma patients across a period of many years.
Patient samples were examined using advanced technologies, known as T cell receptor sequencing and single-cell RNA sequencing.
The studies were completed with a subset of T cells known as “CD8” or cytotoxic T cells. Following this, Turk and Angeles want to find out if analogous traits are observed in patient-helper or “CD4” T cells, and whether similar immunity is produced in patients suffering from skin inflammation apart from vitiligo, like a rash.
The researchers will study how different kinds of immunotherapy influence the population of new cells discovered by them.
Finding that T cells can persist for years throughout skin and blood and understanding what defines such durable immune responses in melanoma patients will lead to better design of therapies to achieve such responses.”
Mary Jo Turk, PhD, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center
Source:
Journal reference:
Han, J., et al. (2021) Resident and circulating memory T cells persist for years in melanoma patients with durable responses to immunotherapy. Nature Cancer. doi.org/10.1038/s43018-021-00180-1.