A new research work, published in JCI - The Journal of Clinical Investigation, has discovered that the endoplasmic reticulum of a neutrophil becomes stressed in the autoimmune disorder lupus. The endoplasmic reticulum is the organelle that usually produces proteins in the cell.
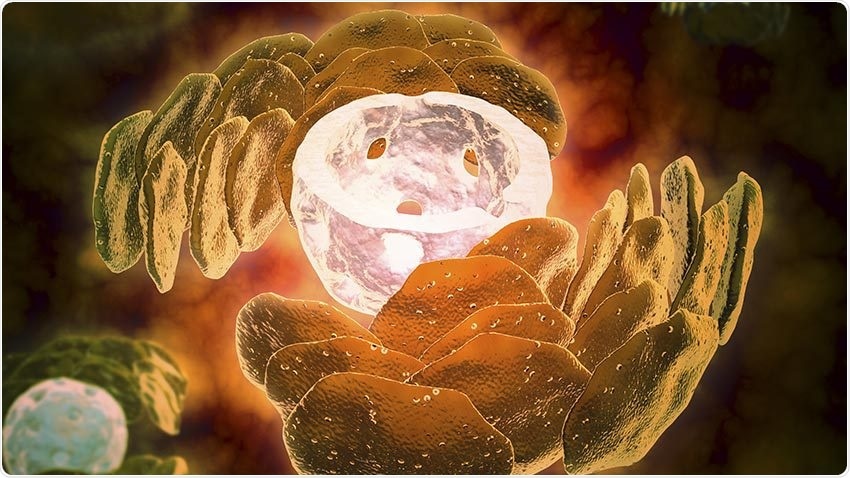
Image Credit: Getty Images.
This stress stimulates a molecule, known as IRE1α, which seems to play a crucial role in the pathogenesis of lupus in mice.
Now, a multidisciplinary research team from the University of Michigan, covering rheumatology, microbiology, and dermatology has found that IRE1α controls the discharge of neutrophil extracellular traps, also called NETs, from lupus neutrophils. These NETs are sticky, spiderweb-like structures that lead to inflammation when released in the wrong place or at the wrong time.
NETs also play a crucial role in the pathogenesis of various autoimmune diseases, including lupus, by inducing the formation of autoantibodies and causing the clotting of blood vessels and damage.
Based on a previous research work conducted by study authors Basel Abuaita, PhD. and Mary X. O'Riordan, Ph.D., as well as immunologists and microbiologists from Michigan Medicine, the researchers were aware that the IRE1α pathway was essential for neutrophil stimulation in models of another potentially dangerous disease, that is, Staphylococcus aureus infection.
Given that neutrophils are over-activated in lupus, we hypothesized that the IRE1α pathway might be part of the story in this disease, too. It’s what prompted this collaboration, and the result was the discovery of an abnormally activated IRE1α pathway in lupus patient neutrophils, which tracks closely with disease severity.”
Gautam Sule, PhD, Postdoctoral Fellow, Rheumatology, Michigan Medicine
But this new research work presented unique difficulties because neutrophils are difficult to study, according to the study author Jason S. Knight, MD, Ph.D., a rheumatologist from Michigan Medicine.
Although neutrophils are the most common white blood cells in circulation, they’re hard to work with in the laboratory because they don’t live long and there isn’t a good cell line system to replicate their functions.”
Jason S. Knight, MD, PhD, Study Author and Rheumatologist, Michigan Medicine
This required the researchers to purify neutrophils from the human blood on a regular basis for their studies, but fortunately, their effort paid off.
The researchers have now a better understanding of neutrophil biology in lupus, but according to them, there is still more work to be done and the following steps will include a study of a wider population of lupus patients, and probably other associated diseases, like antiphospholipid syndrome.
This was a great partnership of basic cell biologists and translational scientists. This project wouldn’t have been possible if either one of our groups had tried to go at it alone. We’re lucky to be at a place like U-M where these partnerships are not only possible but actively encouraged.”
Jason S. Knight, MD, PhD, Study Author and Rheumatologist, Michigan Medicine
Source:
Journal reference:
Sule, G., et al. (2021) Endoplasmic reticulum stress sensor IRE1α propels neutrophil hyperactivity in lupus. JCI - The Journal of Clinical Investigation. doi.org/10.1172/JCI137866.