SARS-CoV-2, the coronavirus responsible for COVID-19, hijacks human cell machinery to disrupt the immune response, enabling it to cause infection, replicate, and cause disease, according to a research team from the University of California San Diego School of Medicine.
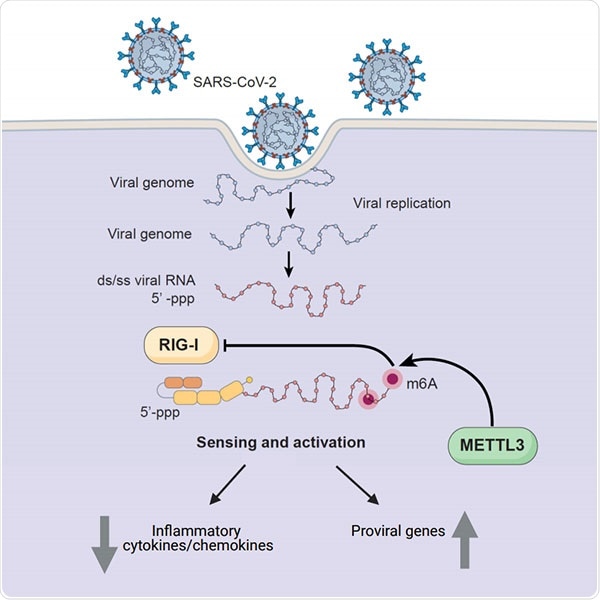
Human enzyme METTL3 adds methyl groups to introduce m6A in SARS-CoV-2’s RNA. That modification prevents the virus’ RNA from triggering inflammatory molecules known as cytokines. METTL3 also leads to increased expression of pro-viral genes — those that encode proteins needed for SARS-CoV-2 replication and survival. Image Credit: University of California San Diego Health Sciences.
In brief, a human enzyme tags the genome of the virus with a special marker that instructs the immune system to rest while increasing production of the surface proteins that SARS-CoV-2 uses as a “doorknob” to penetrate cells.
Published in Cell Reports on April 22nd, 2021, the research paves the way for new anti-viral immunotherapies, which act by strengthening a patient’s immune system instead of directly destroying the virus.
It’s very smart of this virus to use host machinery to simultaneously go into stealth mode and get inside more cells. The more we know about how the virus establishes itself in the body, the better equipped we are to disrupt it.”
Tariq Rana, PhD, Professor and Chief, Division of Genetics, Department of Pediatrics, School of Medicine, University of California San Diego and Moores Cancer Center
Genes (DNA) in human cells are transcribed into RNA, which is then converted into proteins—the molecules that constitute the bulk of cells. However, this is not always so easy. To impact protein production, cells may chemically alter RNA.
The addition of methyl groups to adenosine, one of the building blocks of RNA, is one of these modifications. This alteration, called N6-methyladenosine (m6A), is widespread in humans and other organisms, like viruses.
When compared to humans, the whole genomes of certain viruses, like SARS-CoV-2, are made up of RNA rather than DNA. Instead of transporting the machinery used to convert this into proteins, the coronavirus employs human cells to do the task.
Previously, Rana and his colleagues found that m6A plays a significant role in Zika and HIV infections. The researchers found that the human enzyme METTL3 binds methyl groups to SARS-CoV-2 RNA to introduce m6A.
This change inhibits the RNA of the virus from activating inflammatory molecules called cytokines. Surprisingly, METTL3 activity also induced the expression of pro-viral genes, which encode proteins required for SARS-CoV-2 survival and replication, like ACE2, the cell surface receptor used by the virus to invade human cells.
It remains to be seen why our cells help the virus out like this.”
Tariq Rana, PhD, Professor and Chief, Division of Genetics, Department of Pediatrics, School of Medicine, University of California San Diego and Moores Cancer Center
When the researchers used gene silencing or other approaches to eliminate METTL3 from cells in the lab, they discovered the opposite—a pro-inflammatory molecule called RIG1 binds the viral RNA, more inflammatory cytokines are formed, and pro-viral genes are blocked. Finally, suppressing METTL3 inhibited viral replication.
To observe how this process works in real life, the researchers compared post-mortem lung specimens from COVID-19 patients to healthy lung biopsies.
The team discovered that METTL3 expression was lower and inflammatory genes were increased in patients who died from acute COVID-19. This makes sense in the later stages of COVID-19, according to Rana, because cytokine storm—the overactivation of the patient’s own immune system—is believed to intensify the disease.
It’s like there are two phases of the infection—in the first, the virus needs METTL3 to help it evade the immune response, but in the second phase, once the virus is replicating like crazy, it’s better to downregulate METTL3.”
Tariq Rana, PhD, Professor and Chief, Division of Genetics, Department of Pediatrics, School of Medicine, University of California San Diego and Moores Cancer Center
Rana’s group is now verifying their results in animal models and creating METTL3 inhibitors for testing as future COVID-19 experimental therapies.
“We hope that by manipulating m6A levels in the virus, we might be able to time the innate immune response in a way that benefits patients with COVID19, especially for the mild or moderate patients who haven’t developed cytokine storm. The challenge is that cells have many other enzymes like METTL3, known as methyltransferases, so inhibiting it would need to be done very specifically, at a specific time,” concluded Rana.
Source:
Journal reference:
Li, N., et al. (2021) METTL3 regulates viral m6A RNA modification and host cell innate immune responses during SARS-CoV-2 infection. Cell Reports. doi.org/10.1016/j.celrep.2021.109091.