A promising treatment for melanoma and other types of cancers is neoadjuvant immune checkpoint blockade (ICB). This therapy has been recently demonstrated to offer a modest survival benefit for patients suffering from recurrent glioblastoma.
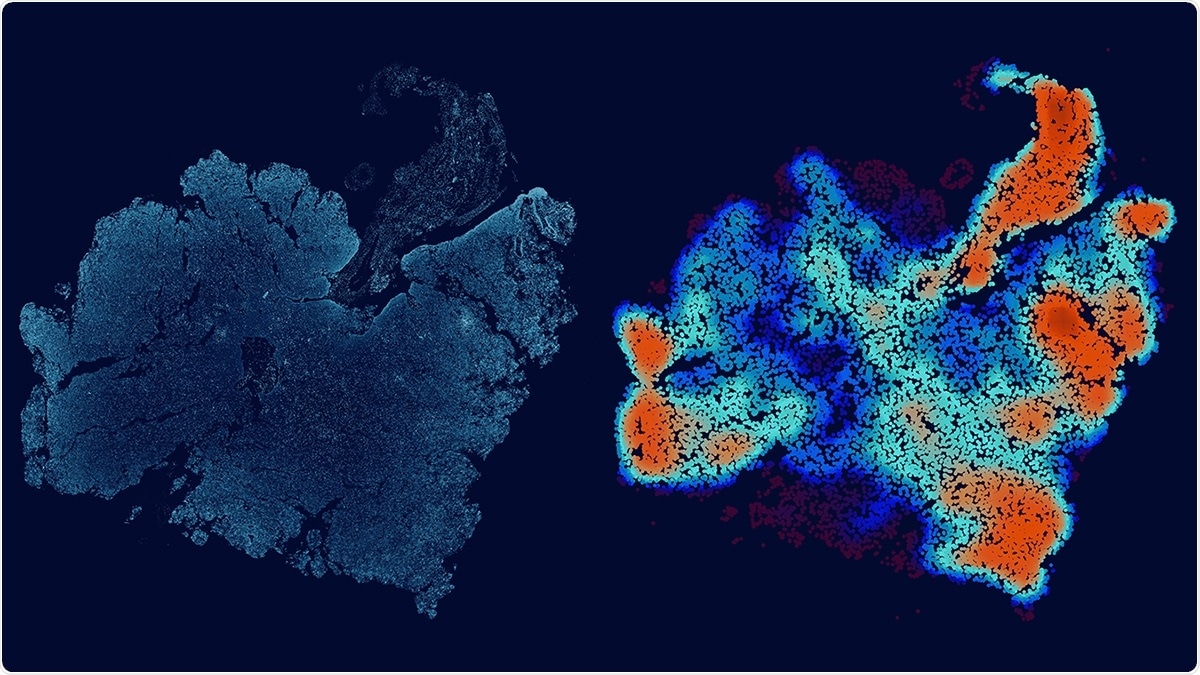
This image depicts a glioblastoma tumor slice and its corresponding immune-cell density map. Image Credit: Allison Kudla, PhD/ISB.
To enhance the efficacy of this treatment, researchers are searching for vulnerabilities in glioblastoma tissues that have been removed surgically. However, this has proved to be rather difficult because of the huge differences between patients and within the tumor.
To deal with this challenge, the team from the Institute for Systems Biology (ISB) along with their colleagues came up with a new way to analyze tumors. This technique uses machine-learning-based image analysis as well as multiplex spatial protein profiling of microscopic compartments in the tumor to build mathematical models.
Using this approach, the researchers compared and analyzed the tumor tissues obtained from 23 patients with high-risk melanoma and 13 patients with recurrent glioblastoma. Both groups of patients were treated with neoadjuvant ICB.
The researchers used melanoma to guide the understanding of glioblastoma analyses and subsequently identified the proteins that correspond with tumor growth, tumor-killing T cells, and immune cell-cell interactions.
This work reveals similarities shared between glioblastoma and melanoma, immunosuppressive factors that are unique to the glioblastoma microenvironment, and potential co-targets for enhancing the efficacy of neoadjuvant immune checkpoint blockade.”
Dr Yue Lu, Study Co-Lead Author, Institute for Systems Biology
Dr. Alphonsus Ng, also the study co-lead author, stated, “This framework can be used to uncover pathophysiological and molecular features that determine the effectiveness of immunotherapies.”
Recently published in the Nature Communications journal, the study is a joint project by ISB, UCLA, and MD Anderson. Brain cancer is one of the most challenging settings for realizing immunotherapy success. This successful association between clinicians and scientists provides an excellent opportunity to improve patient care and gain a better understanding of cancer immunotherapy at the deepest levels.
We believe that the integrated biological, clinical and methodological insights derived from comparing two classes of tumors widely seen as at the opposite ends of the spectrum with respect to immunotherapy treatments should be of interest to broad scientific and clinical audiences.”
Dr Jim Heath, Study Corresponding Author and President, Institute for Systems Biology
Source:
Journal reference:
Lu, Y., et al. (2021) Resolution of tissue signatures of therapy response in patients with recurrent GBM treated with neoadjuvant anti-PD1. Nature Communications. doi.org/10.1038/s41467-021-24293-4.