Similar to how a spider traps its prey, the cells of the human immune system cooperate to trap and “eat” bacteria.
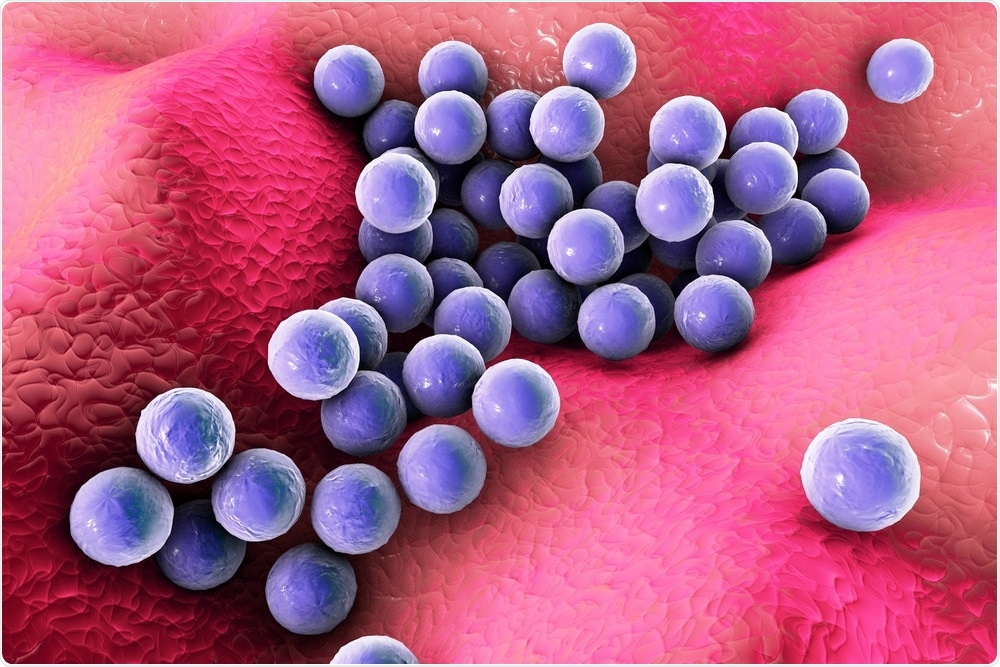
Image Credit: Kateryna Kon/Shutterstock.com
The antibacterial mechanism identified recently and reported in Science Advances on September 10th, 2021, could pave way for innovative approaches to combat Staphylococcus aureus (staph) and other extracellular bacterial pathogens.
Neutrophils, or the first responder immune cells that migrate to infection sites, are known to self-destruct and discharge their protein and DNA contents to produce neutrophil extracellular traps (NETs). Vanderbilt researchers headed by postdoctoral fellow Andrew Monteith, Ph.D., have now identified that NETs promote the bacterial killing power of another type of immune cell: macrophages.
“Neutrophils produce the spider webs that immobilize the bacteria, and macrophages are the spiders that engulf and kill the bacteria,” stated Eric Skaar, Ph.D., MPH, Ernest W. Goodpasture Professor of Pathology, Microbiology, and Immunology and director of the Vanderbilt Institute for Infection, Immunology, and Inflammation.
Staph bacteria, specifically antibiotic-resistant strains, are a major cause of hospital-acquired infections, pus-forming skin and soft tissue infections, and infectious heart disease.
Neutrophils and macrophages—both phagocytic cells—are known for consuming bacteria and generating antimicrobial peptides, reactive oxygen species, and other enzymes to combat infection.
According to Skaar, NET generation, or NETosis that is considered to be a kind of programmed cell death, is a more recently identified neutrophil antibacterial approach. The discharged neutrophil DNA forms a sticky trap that is also filled with antimicrobial peptides.
Monteith and his team used neutrophils that experience increased NETosis in animal and in vitro model systems to analyze the biological function of NETs. They identified that increased NETosis did not offer a killing advantage to neutrophils in isolation.
However, in the presence of macrophages, NET formation improved macrophage antibacterial activity by increasing phagocytosis—of staph bacteria trapped in the NETs along with neutrophil antimicrobial peptides.
The macrophages end up with not only their own antibacterial arsenal, but also the neutrophils’ antibacterial arsenal, all in the same compartment killing the bacteria.”
Eric Skaar, Ernest W. Goodpasture Professor of Pathology, Microbiology and Immunology and Director, Vanderbilt Institute for Infection, Immunology and Inflammation
Higher NET generation also promoted macrophage killing of other bacterial pathogens such as Streptococcus pneumoniae and Pseudomonas aeruginosa. The study results indicate that neutrophil/NET-macrophage cooperation is a widely used immune defense mechanism.
The team also demonstrated that the removal of a staph nuclease enzyme that cuts DNA makes the bacteria much more sensitive to NET-macrophage killing.
It seems as if extracellular pathogens like staph have evolved secreted nucleases so they can cut their way out of these NETs—chop off the spider web and escape.”
Eric Skaar, Ernest W. Goodpasture Professor of Pathology, Microbiology and Immunology and Director, Vanderbilt Institute for Infection, Immunology and Inflammation
When the nuclease is blocked, the pathogens become more vulnerable to NET-mediated killing and it may be a good antibacterial treatment approach. This king of “anti-virulence” approach would enable phagocytic and other immune cells to perform their roles and kill the bacteria, added Skaar.
Scientists are excited about the idea of anti-virulence strategies, because we know a lot about bacterial virulence mechanisms and can come up with creative ways to inhibit them.”
Eric Skaar, Ernest W. Goodpasture Professor of Pathology, Microbiology and Immunology and Director, Vanderbilt Institute for Infection, Immunology and Inflammation
However, existing pharmaceutical efforts focus only on drugs that directly destroy bacteria instead of blunting their virulence.
Monteith, Skaar, and the team are continuing to investigate NETosis, such as how and when neutrophils opt for this form of cell death. They also seek to know how individual differences in NETosis—may be due to genetic variation or disease states—influence infection. For instance, in people with specific autoimmune conditions, decreased NETosis may increase the vulnerability to staph infections.
Source:
Journal reference:
Monteith, A. J., et al. (2021) Neutrophil extracellular traps enhance macrophage killing of bacterial pathogens. Science Advances. doi.org/10.1126/sciadv.abj2101.