A group of researchers recently discovered a compound that reveals potential in alleviating the symptoms of coronavirus infections while examining a disease caused by a close cousin of the virus behind COVID-19.
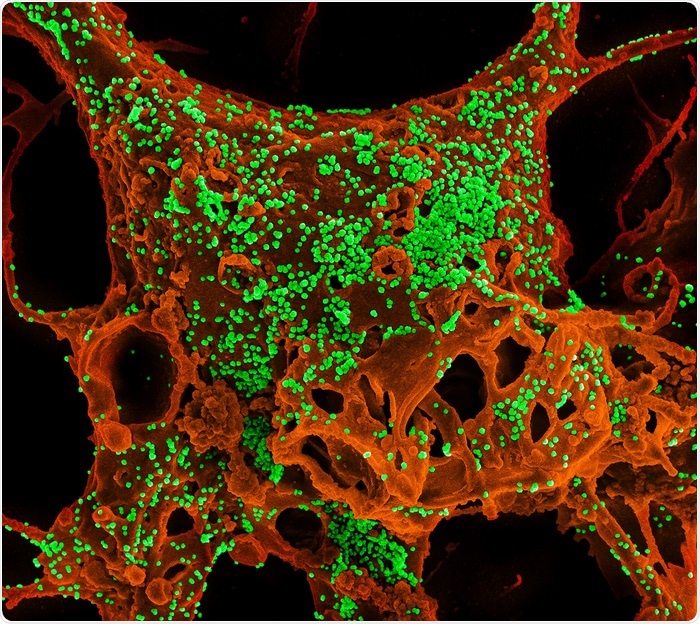
Color-enhanced scanning electron micrograph of mammalian cells infected with Middle East Respiratory Syndrome coronavirus. Image Credit: Photo courtesy of National Institute of Allergy and Infectious Diseases, NIH.
The researchers from the Department of Energy’s Pacific Northwest National Laboratory and the University of North Carolina at Chapel Hill analyzed the virus that causes Middle East Respiratory Syndrome—a coronavirus. MERS is less common and is also more lethal than COVID-19.
The researchers investigated how the virus causing MERS damages the lungs and harms patients. In lab research works, the scientists examined tens of thousands of protein measurements, molecular messengers, and other signals that arise after infection. The scientists identified a molecular mechanism, part of the body’s quality-control machinery, that performs a vital role in causing damage from a coronavirus infection.
The researchers examined a huge database of compounds and pinpointed one—called AMG PERK 44—that hinders virus replication in human tissue under laboratory conditions. The researchers also discovered that this compound has a great effect on mice infected with the virus. The compound enhanced lung function and decreased lung damage and weight loss in the mice, specifically in male mice.
The broad fight against respiratory diseases
Battelle, which operates PNNL, and UNC filed for a patent for using PERK inhibitor to treat coronavirus infections. However, the researchers highlight that it is too soon to determine if the compound can aid patients. PERK inhibitor is not used as a drug at present.
They state that the observations of the study are much useful as part of a wider effort to understand much about respiratory diseases. The research was published in the mBio journal.
“Studies like this help us learn more about how deadly respiratory viruses operate—how they do what they do, why they attack certain parts of the lung and not others,” stated PNNL virologist Amy Sims, one of two first co-authors of the paper, along with PNNL scientist Hugh Mitchell.
Studying how these viruses work helps us understand why patients exhibit the symptoms they do and ultimately how to treat or prevent disease.”
Amy Sims, Study Co-First Author and Virologist, Pacific Northwest National Laboratory
Sims was researching coronaviruses for over 20 years. She and her associates started the present research eight years ago, before the advent of the coronavirus that causes COVID-19. The observations of the research carried out years after Sims and coworkers crafted it can help millions of people infected with SARS-CoV-2, the virus causing COVID-19.
Emergency response—for damaged proteins
The group’s research is directed towards proteins—the workhorses of the body’s cells. Proteins perform various functions to keep organisms, like people, alive and well. The body keeps close tabs on the functioning and intactness of the proteins.
Once the body produces proteins that are not up to standard for reasons, including infection, protein-repair machinery in a cell’s endoplasmic reticulum goes into emergency response mode. The organelle functions like a triage center for damaged proteins during stress.
At the time of swamping with misfolded proteins, the unfolded protein response, or UPR, comes in. The UPR sets a temporary halt to all cellular activity connected to producing new proteins. This makes time for the cell to carry out the needed repairs to misfolded proteins.
When many proteins are damaged and the protein-repair and folding machinery could not recover, the system drives other proteins to destroy the cell. The researchers discovered this system and found that it is very active in specific lung cells when the body responds to a MERS infection.
The current research involved handling of lung tissue and mice at UNC, in a lab led by one of the world’s top coronavirus researchers, Ralph Baric. Researchers at PNNL analyzed and interpreted huge amounts of data on molecular messages. Sims worked in the Baric laboratory while at UNC and joined PNNL earlier last year. The two institutions have worked jointly for years.
Baric says, “Coronavirus infections cause complex disease phenotypes, and new strategies are needed to disentangle which host pathways are contributing to the development of severe, life-threatening outcomes.”
Consider how fast a vaccine to protect against COVID-19 was created and how quickly new drugs were found to treat the disease. The success wasn’t because scientists started from scratch when the virus appeared. They were able to build upon years and years of research understanding how the immune system works and how it responds to coronaviruses. You never know when a certain bit of knowledge will prove crucial in the future.”
Amy Sims, Study Co-First Author and Virologist, Pacific Northwest National Laboratory
Source:
Journal reference:
Sims, A. C., et al. (2021) Unfolded Protein Response Inhibition Reduces Middle East Respiratory Syndrome Coronavirus-Induced Acute Lung Injury. mBio. doi.org/10.1128/mBio.01572-21.