Researchers at Northwestern University have created a new technology that allows them to use immune cells from tumors to combat cancer more quickly and efficiently.
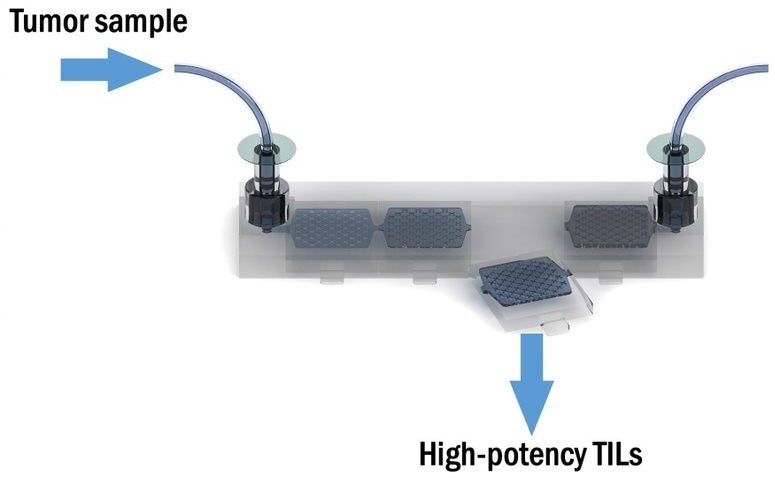
The 3D printable device can be easily reproduced and moved between labs and hospitals. A tumor sample enters the device, and high potency tumor-eating cells are spit out. Image Credit: Northwestern University.
Their findings indicated that when compared to typical cell therapy methods, tumors in mice shrank dramatically. The scientists multiplied, filtered through, and collected hundreds of millions of cells using a unique micro fluidic device that could be 3D printed, recovering 400% more tumor-eating cells than previous methods. The study was published on January 27th, 2022, in the journal Nature Biomedical Engineering.
Toxic chemicals and foreign materials are used in most cancer treatments, causing serious side effects and weakening the immune system. Many disease therapies in regenerative medicine and cancer treatment have picked up steam in the clinic by using tissue from one’s own body, which can avoid side effects and the danger of rejection. However, the wheels do occasionally skid.
People have been cured in the clinic of advanced melanoma through treatment with their own immune cells that were harvested out of tumor tissue. The problem is, because of the way the cells are harvested, it only works in a very small number of patients.”
Shana O. Kelley, Study Corresponding Author and Pioneer, Translational Biotechnology, Northwestern University
Kelley is a professor of biochemistry and molecular genetics at Northwestern University Weinberg School of Medicine and the Neena B. Shwartz Professor of Chemistry and Biomedical Engineering at Northwestern University Weinberg College of Arts and Sciences and McCormick School of Engineering.
Tumor-infiltrating lymphocytes (TILs) are natural immune cells that infiltrate tumor tissue by confronting cells in a type of hand-to-hand warfare that resembles someone spraying insecticide on weeds. However, in this case, researchers have been earlier battling the weeds with a chemical canister that has half-expired.
This is the case with today’s cell therapies, which use a combination of “exhausted” and “naive” cells to cure cancers. Cells are collected from tissue and cultivated in labs far distant from the patients from whom they were taken. Many of the cells are fatigued and therefore unable to fight by the time they have proliferated and are ready to be reintroduced into the body, having spent too much time in the tumor.
Assembling the best fighters
Researchers used cell sorting techniques enabled by nanotechnology to specify which cells are most active using a novel technology called micro fluidic affinity targeting of infiltrating cells (MATIC). The authors of the study employed MATIC to locate the “Goldilocks population” of cells, which produced impressive results for the mice population they were examining.
Tumors in mice reduced dramatically—and in some cases vanished entirely—leading to a significant increase in survival rates when compared to more typical TIL recovery approaches.
Instead of giving mice this mixture of cells with different phenotypes, we’re giving them the one cell phenotype that can actually help them. You see much more potency and a much higher response rate when you really home in on the sweet spot of T cell reactivity.”
Shana O. Kelley, Study Corresponding Author and Pioneer, Translational Biotechnology, Northwestern University
Reproducible, accessible technology
Kelley believes that the 3D-printed gadget might be used in hospitals rather than being kept in a lab, as her team’s invention is compact and easy to replicate. Bringing cell therapy closer to patients will drastically lower research and development costs, allowing the treatment to reach a larger number of people.
Kelley moved to Northwestern from the University of Toronto in August and has continued to research how her platform can help cancer patients. She is now utilizing the gadget to look for the same types of TILs in blood samples, which would remove the requirement for surgery to remove a small portion of a tumor to this type of treatment.
Kelley has started a small firm to commercialize her devices, and she hopes to continue working with industry partners and collaborators at Northwestern to expand the tool’s applications.
The platform has been employed in a variety of applications, the majority of which have included the characterization and measurement of rare cells in the body.
When we take on the development of a new technology, we typically end up with a hammer, and then need to go find a nail. We got introduced to problems in cell therapy, and it was immediately apparent that this was a perfect fit.”
Shana O. Kelley, Study Corresponding Author and Pioneer, Translational Biotechnology, Northwestern University
Source:
Journal reference:
Wang, Z., et al. (2022) Efficient recovery of potent tumor-infiltrating lymphocytes through quantitative immunomagnetic cell sorting. Nature Biomedical Engineering. doi.org/10.1038/s41551-021-00820-y.