Most people’s immune responses are powerful enough to prevent the SARS-CoV-2 virus from spreading throughout the body that they are immune to pneumonia. However, experts have been stumped as to how the intruder is confined in the upper respiratory system.
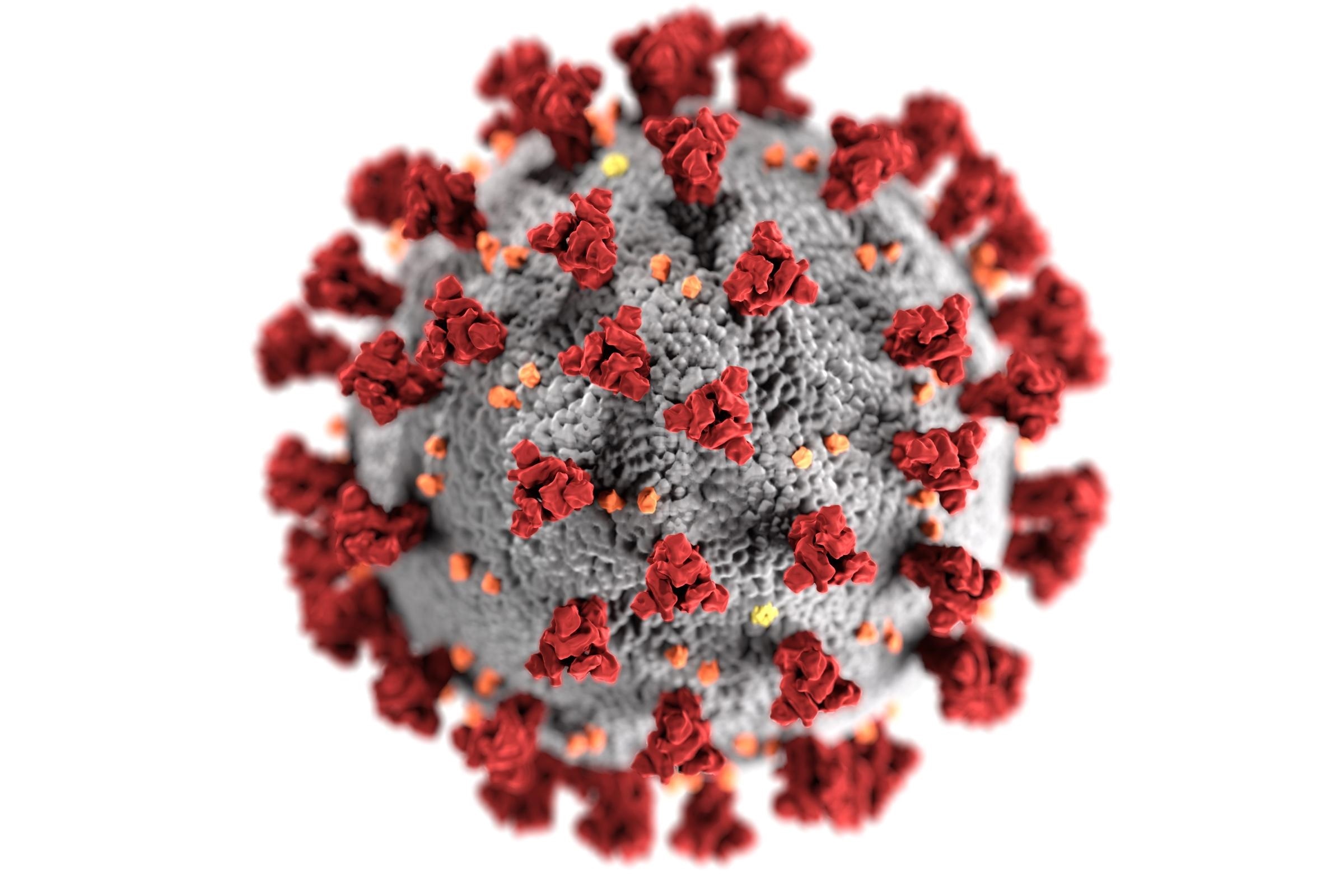
Image Credit: Ludwig-Maximilians-Universität München.
Working in collaboration with other research institutions, scientists at LMU’s University of Munich Hospital, led by Dr med. Kami Pekayvaz, Alexander Leunig, Associate Professor Dr med. Konstantin Stark, and Dr med. Leo Nicolai discovered that people with mild disease classes had a particular, specific antiviral increase in the levels of so-called interferon-stimulated genes.
According to current studies, 90% of SARS-CoV-2 infected people can effectively fight the virus, preventing a serious infection of the lungs. To figure out how this occurs, the researchers looked at blood samples and nose swabs from over 100 individuals, using a variety of methodologies to analyze genes, proteins, and other components involved in the immune response. Researchers paired their findings with clinical evidence already available.
The study’s major goal was to look at patient samples throughout the disease. First, the scientists intensively observed and studied a group of patients with risk indicators for a serious course of the disease, differentiating between those with and without respiratory involvement. The results were subsequently confirmed in a large population of outpatients with modest disease progression.
Authors from the Medical Clinic and Polyclinic I located in the Munich district of Großhadern added, “We discovered that early on in the disease, patients who had hardly any or no symptoms at all exhibited a very strong antiviral response in the immune cells in the blood. You can picture these as a whole arsenal of proteins that cells can use against viral intruders.”
The authors added, “We think that this type of immune response prevents further spread of the virus, as the body is put on alert, meaning for example that the lung tissue is prepared for the intruder.”
Upregulation of interferon-stimulated genes characterizes the response (ISGs). Furthermore, so-called natural killer cells and T cells appear to be less hostile against other cells in moderate instances. This is most likely to keep the body’s cells from being injured. Finally, an anti-inflammatory monocyte signature was found, which is indicative of a protective response.
In conclusion, the scientists noted to have discovered a “specific immunological signature” that can stop the SARS-CoV-2 virus from propagating throughout the body. Surprisingly, this immune response is independent of antibodies at first, as they are formed later in the disease.
“One goal now would be to modulate the immune system of high-risk patients or of individuals after viral exposition to activate these antiviral mechanisms. Approaches already exist towards this—for example, nasal sprays have been used that trigger such a response via interferon alfa or other mechanisms,” concluded authors.
The scientists argue that these tactics should now be improved, emphasizing that such promising strategies might potentially be useful in the future pandemic against viruses other than SARS-CoV-2.
Source:
Journal reference:
Pekayvaz, K., et al. (2022) Protective immune trajectories in early viral containment of non-pneumonic SARS-CoV-2 infection. Nature Communications. doi.org/10.1038/s41467-022-28508-0.