People who developed immunity to SARS-CoV-2, the virus that can cause COVID-19, either by vaccination or contact, are expected to get some protection against the pathogen’s omicron version.
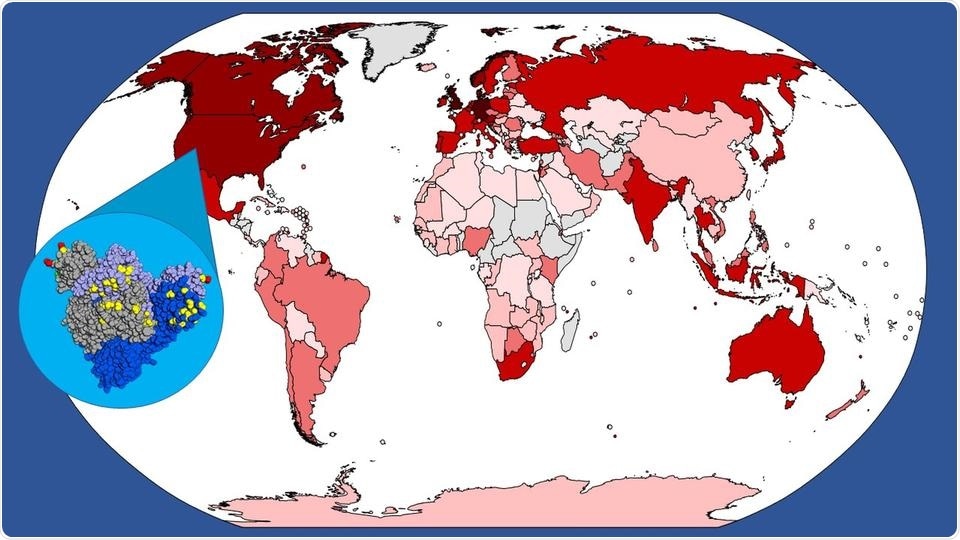
A world map showing confirmed cases of COVID-19 caused by the omicron variant of SARS-CoV-2 as of February 11th, 2022, with darker colors indicating higher case counts. The inset is a color-coded map of mutations (yellow, red, and green sections) identified in the omicron variant spike protein. A Johns Hopkins Medicine study shows these mutations—that led to the omicron variant—did not help it escape recognition by T lymphocyte immune cells. Image Credit: Graphic created by M.E. Newman, Johns Hopkins Medicine, using public domain images.
According to an international research team led by Johns Hopkins Medicine in partnership with the National Institute of Allergy and Infectious Diseases (NIAID) and ImmunoScape, a US–Singapore biotechnology company, the mutations that resulted in the variant’s emergence are not noticed in the regions of the virus that enhance one form of the cellular immune response.
Moreover, the researchers point out that their study results only apply to one form of cell-mediated immunity—the body’s fight against invaders which does not constitute circulating antibodies—and it is possible that when omicron causes so-called groundbreaking infections, it is the antibody-related immune response (known as humoral immunity) that neglects.
The work was published in mBio, a publication of the American Society for Microbiology, on March 1st, 2022.
We found in a January 2021 study that in people previously infected with the original COVID strain, specific epitopes [portions of a protein that elicit an immune response] from the virus are recognized by immune system cells known as CD8+ T lymphocytes or killer T cells and that this recognition enables a cell-mediated attack on COVID.”
Andrew Redd, Study Lead Author and Assistant Professor, Medicine, Johns Hopkins University School of Medicine
Andrew Redd, who is also a staff scientist at the National Institute of Allergy and Infectious Diseases noted, “In our latest work, we found that these epitopes remained virtually untouched by the mutations found in the omicron variant. Therefore, the CD8+ T cell response to omicron should be virtually as strong as it was to the initial form of SARS-CoV-2.”
People who were previously infected with or vaccinated against the initial SARS-CoV-2 strain have shown remarkably comparable outcomes in other study groups in the United States and South Africa.
Killer T cells (also termed cytotoxic T cells) are CD8+ T cells that can destroy foreign invaders such as viruses and bacteria from the body. T cells were obtained from blood samples taken in 2020 from 30 individuals who had been cured from mild to moderate COVID-19 infections.
According to Redd, the convalescent plasma donors contained six human leukocyte antigens (cell-surface proteins that govern the immune system and are components of each person’s genetic sequence) that were typical of more than 73 percent of the population in the United States.
This suggests that a significant portion of Americans who have been vaccinated against or exposed to the original strain of SARS-CoV-2 might have cytotoxic T cells that can produce an immune response to omicron.”
Aaron Tobian, Study Senior Author and Director, Transfusion Medicine Division
Aaron Tobian is also a professor of Pathology at Johns Hopkins University School of Medicine
The blood samples utilized in this study were taken from 26–62 days after the donors ceased reporting COVID-19 symptoms, and were originally obtained for the research team’s prior investigation of immune response in recovered patients. This allowed the donors’ immunological responses to the virus to mature to the point where CD8+ T cells were ready to fight it. After the researchers measured the T cell response, the samples were preserved.
Donor samples were submitted to ImmunoScape for the challenging task of determining which T cells had reacted to SARS-CoV-2 during that examination. The company’s deep immune cell profiling technology, in particular, revealed which viral proteins provoked a T cell-directed response—information that might shed light on T cells’ functional features.
Blood samples were examined with 408 distinct SARS-CoV-2 epitopes comprising spikes on the viral surface, the virus capsule, and nonstructural proteins within the virus in the initial investigation. T cells from convalescent donors identified 52 of the 408 epitopes, according to the researchers.
According to Redd, the researchers analyzed the 52 epitopes previously found in convalescent blood samples to see if they had been changed by escape mutations, which are genetic modifications that allow the virus to evade being sensitive to cell-mediated immunity.
We only found one low-prevalence epitope from the omicron spike protein that had a minor change from its predecessor in the original virus. Overall, the omicron variant is known to have some 50-plus mutational differences between it and the original SARS-CoV-2 strain, but it seems the virus has not evolved the ability to avoid T cell recognition.”
Andrew Redd, Study Lead Author and Assistant Professor, Medicine, Johns Hopkins University School of Medicine
While considerable cell-mediated immunity seems to have been preserved from the original SARS-CoV-2 through its variations, Redd, Tobian, and their collaborators believe the additional investigation is required to properly understand why people who have this protection can still become sick with omicron.
Source:
Journal reference:
Redd, A. D., et al. (2022) Minimal Crossover between Mutations Associated with Omicron Variant of SARS-CoV-2 and CD8+ T-Cell Epitopes Identified in COVID-19 Convalescent Individuals. mBio. doi.org/10.1128/mbio.03617-21.