One in every two people will acquire cancer at some point in their lives, according to the most recent international estimate. Blood malignancies, as well as other previously uncommon cancer types, are becoming more widespread in the population. Rare cancer research is crucial not only for bettering the treatment of those who have them but also for teaching about what makes other tumors susceptible.
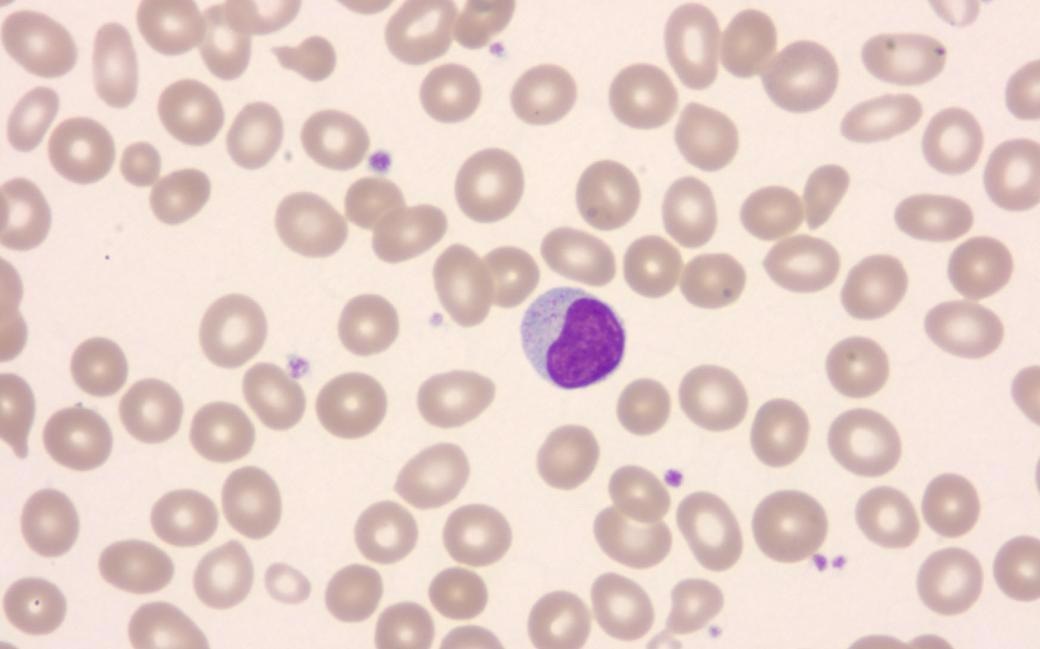 LGL-leukemia cell. Image Credit: Dr. Claudiu Cotta
LGL-leukemia cell. Image Credit: Dr. Claudiu Cotta
Large granular lymphocyte (LGL) leukemia is an uncommon type of blood cancer in which cancer cells are formed by the body's immune cells, T cells. Although LGL leukemia is rarely fatal, it does induce several long-term symptoms, including a greater risk of infection, anemia, and joint discomfort.
The LGL cancer cells are assumed to be targeting the body’s tissues, causing the symptoms. In reality, LGL leukemia has a lot in common with autoimmune disorders. The majority of current treatments are ineffective, and patients’ symptoms recur shortly.
Our research group demonstrated 10 years ago that LGL cancer cells typically have a mutation in the STAT3 gene, a finding that is now used to diagnose this disease worldwide.”
Satu Mustjoki, Professor, Translational Hematology, University of Helsinki
“Researchers have previously analyzed primarily LGL cancer cells, but we wondered whether other cells of the patient’s immune system could also have a role in this disease,” comments Doctoral Researcher Jani Huuhtanen, LicMed, from the University of Helsinki and Aalto University.
Technical research solutions and research datasets in a key position
Conventional methods for distinguishing immune system cells from blood cancer cells have proven to be particularly challenging, according to the researchers, because cancer cells in LGL leukemia, for example, bore a striking resemblance to normal T cells found in the blood.
Researchers have been able to analyze individual cells one at a time, thanks to a breakthrough in single-cell procedures. The scientists were able to isolate cancer cells from normal T cells and evaluate them for the first time using these approaches.
Single-cell techniques open up entirely new avenues for research.”
Tiina Kelkka, Docent, Immunology, University of Helsinki
“But we still needed a large patient cohort, which is hard to gather in rare diseases. Thanks to our research group’s international collaboration network, we were able to compile a dataset of almost 200 LGL leukemia patients’ samples from Finland, Germany, Italy, the USA, and Japan,” she adds.
Locking on the immune system and novel therapies
The research, which used this large dataset, confirmed the group’s assumptions: in LGL leukemia, the entire immune system, not just the LGL cancer cells, is different from other cancers.
The immune system in these patients is overactivated and keeps giving the tumor cells cues to keep growing as well as provides them with a favorable environment.”
Dipabarna Bhattacharya, Doctoral Researcher, University of Helsinki
To improve patients’ quality of life, existing medicines for LGL leukemia should target the entire immune system, not just the cancer cells, according to the research.
“We believe that similar findings will be made in other cancers. In fact, our goal is to use the same techniques to decipher the role of the immune system in other cancers too,” Jani Huuhtanen concludes.
Source:
Journal reference:
Huuhtanen, J., et al. (2022) Single-cell characterization of leukemic and non-leukemic immune repertoires in CD8+ T-cell large granular lymphocytic leukemia. Nature Communications. doi.org/10.1038/s41467-022-29173-z.