Treatment with chimeric antigen receptor T cells (CAR T cells) is often the last hope for patients with lymphoma, multiple myeloma, or certain kinds of leukemia. T cells from the patient’s blood are extracted and artificial receptors—the CARs—are added to them in the lab.
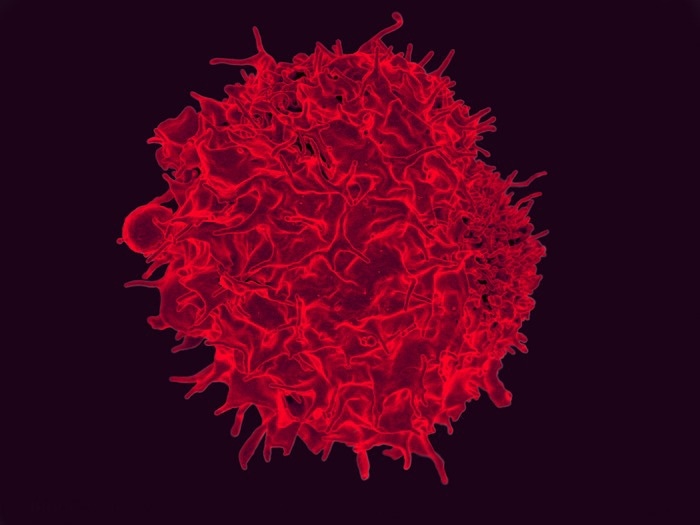 Colorized scanning electron micrograph of a T lymphocyte. Image Credit: NIAID
Colorized scanning electron micrograph of a T lymphocyte. Image Credit: NIAID
T cells, the guardians of the immune system, are constantly on the lookout for foreign structures in blood vessels and tissues. T cells that have CARs can detect very specific surface structures on cancer cells. When the CAR T cells are infused back into the patient, they flow freely in the body as a kind of living drug that can attach to and kill very specific tumor cells.
The crafted immune cells live in the body indefinitely and multiply. They will return to action if cancer returns. At least, that is the theory. In practice, however, many patients relapse. This is due to tumor cells’ ability to outwit CAR T cells by generating more of the protein EBAG9 and affecting the T cells to produce more of it as well. EBAG9 inhibits the secretion of cytotoxic enzymes in T cells, slowing the preferred immune response.
A month earlier, a team headed by last authors Dr Armin Rehm and Dr Uta Höpken from the Helmholtz Association’s Max Delbrück Center for Molecular Medicine (MDC) demonstrated in the journal JCI Insight that closing down the EBAG9 gene in mice resulted in a long-term increase in the immune response to cancer.
In addition, the mice evolved more T-memory cells. These cells are part of human immunological memory, which enables the immune system to respond more effectively to a cancer antigen after initially experiencing it.
Now scientists have also revealed these significant findings in vitro, in human CAR T cells. Writing in Molecular Therapy, the team says that this is the key step on the road to therapeutic use.
Shutting down EBAG9 allows the body to eradicate tumor cells earlier and more radically. As well as achieving longer-lasting therapeutic success, this could also create a real chance of cure.”
Dr Armin Rehm, Study Last Author, Max Delbrück Center for Molecular Medicine, Helmholtz Association
Releasing the brake for immunotherapy
Researchers recognized the importance of the EBAG9 gene in cancer as soon as it was discovered. However, it took a very long time to figure out what that role was. When the MDC team began working on it in 2009, they discovered that mice lacking the gene fared much better against bacterial and viral infections and that they established more T-memory cells, which are of specific importance in tumor biology.
Then, in 2015, lead author Dr Anthea Wirges used microRNA to inhibit EBAG9 protein synthesis. She used microRNA to nurture “EBAG9-silenced” CAR T cells with various human leukemia or lymphoma cells for the latest study. Similarly, to the mouse model, silencing significantly reduced tumor growth. Relapses appeared much later as well.
Releasing the EBAG9 brake allows the genetically engineered T cells to release more cytotoxic substances. However, they don’t cause the strong cytokine storm that is typically a side effect of CAR therapy. Switching off the immune brake works across the board. We can do it with every CAR T cell that we produce—regardless of which type of blood cancer it targets.”
Dr Anthea Wirges, Study Lead Author, Max Delbrück Center for Molecular Medicine, Helmholtz Association
Since fewer cells are used, the risk is reduced.
Clinical studies are the next step
However, chemotherapy coupled with conventional antibody therapy will continue to be the first-line therapy for blood cancer because many patients react well to it.
“CAR therapy only comes into play if cancer returns. It’s very expensive because it’s an individual cellular product for a single person,” says Höpken. In addition, a single treatment with that product can save a life.
The EBAG9 work demonstrates the importance of patience and perseverance for scientists. Wirges was inspired by the potential outcome of her work being clinically applicable.
“Projects like this allow you to get to grips with a technique in basic research and then apply everything in translational research—right up to toxicological screening for the regulatory processes,” Rehm adds.
Their project has now entered the final stage: the researchers will discuss their concept with Germany’s biologics approval agency, the Paul Ehrlich Institute, in November.
The team now knows that distributing the EBAG9 brake is extremely effective and has no more adverse effects than traditional CAR T therapy, thanks to their findings from animal models and in vitro experiments using human cells.
“We now need bold clinicians and a partner for financing the clinical studies,” says Rehm. If all goes well, EBAG9-silenced CAR T cell therapy could be accessible to patients in less than two years.
Source:
Journal reference:
Wirges, A., et al. (2022) EBAG9-silencing exerts an immune checkpoint function without aggravating adverse effects. Molecular Therapy. doi.org/10.1016/j.ymthe.2022.07.009.