The treatment of various tumors has been transformed by cell-based immunotherapy, often known as CAR-T cell therapy. To target and combat specific forms of leukemia and lymphoma, the treatment employs genetically engineered T cells.
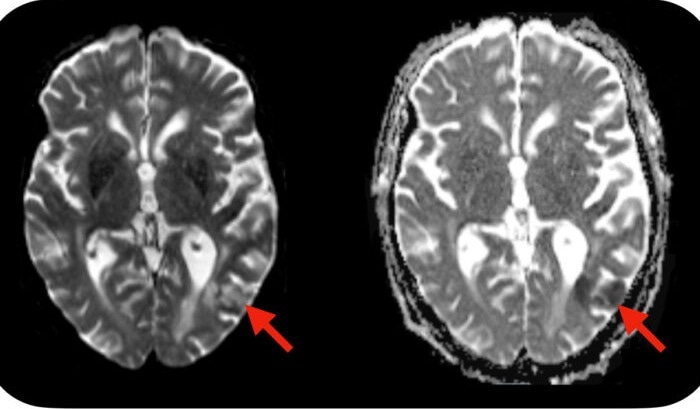 A new study from Washington University School of Medicine in St. Louis suggests a simple blood test—administered before CAR-T cell treatment is initiated—may identify which patients are predisposed to developing neurotoxic side effects after CAR-T cell therapy. Severe side effects can include seizures, brain swelling and strokes. Evidence of a stroke (red arrows) is seen on this MRI scan of the brain of a patient who developed neurotoxic side effects after CAR-T cell therapy. Image Credit: Duke University
A new study from Washington University School of Medicine in St. Louis suggests a simple blood test—administered before CAR-T cell treatment is initiated—may identify which patients are predisposed to developing neurotoxic side effects after CAR-T cell therapy. Severe side effects can include seizures, brain swelling and strokes. Evidence of a stroke (red arrows) is seen on this MRI scan of the brain of a patient who developed neurotoxic side effects after CAR-T cell therapy. Image Credit: Duke University
While it has the potential to cure cancer in certain individuals who would otherwise pass away from the disease, it also carries the danger of a number of adverse effects, some of which can be fatal and disrupt brain function.
According to a recent study from Washington University School of Medicine in St. Louis, a quick blood test could help doctors determine which patients are more likely to experience neurotoxic side effects in the days and weeks following CAR-T cell therapy.
Researchers discovered that levels of a protein called neurofilament light chain (NfL) are higher in individuals who go on to have neurotoxic problems after studying blood samples taken from patients before, during, and after CAR-T cell therapy. Before the therapy even starts, there are high quantities of the protein present, and those levels stay high throughout the therapy and for up to a month after.
The study, published on September 1st, 2022, in the journal JAMA Oncology, may assist medical professionals to foresee these potentially fatal side effects and enable them to start administering medications that can lessen the neurotoxic consequences early on in a patient’s treatment. Additionally, it provides a platform for early CAR-T cell treatment side effect prevention or risk reduction research.
Our study suggests that some patients receiving CAR-T cell therapy have previously undetected damage to neurons present at baseline, before we even begin preparing them for this treatment. We don’t know the origin of this damage, but it appears to predispose them to developing neurotoxic complications. If we understand who is at risk of these complications, we can take early steps to prevent it or reduce the severity.”
Omar H. Butt, MD, PhD, Study Lead Author and Instructor, Medicine, Washington University School of Medicine in St. Louis
Omar H. Butt treats patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.
The NfL protein, a broad indicator of neuronal damage, has been used to gauge or track the severity of a number of neurological conditions, including Alzheimer’s disease and multiple sclerosis.
Measures of NfL in the blood are being used as a way to evaluate the effectiveness of potential new therapies for multiple sclerosis.”
Beau M. Ances, MD, PhD, Study Co-Senior Author and Daniel J. Brennan Professor, Neurology, Washington University School of Medicine in St. Louis
Beau M. Ances adds, “We plan to continue our studies to find the origin of neuronal damage in these cancer patients. This is a unique collaboration that was possible at Washington University because we have some of the top experts in CAR-T cell therapy and leading expertise in neurodegenerative diseases. It presents a great opportunity to bridge gaps and bring these fields together to try to solve a vexing problem and help patients.”
Thirty individuals underwent treatment at Siteman Cancer Center and Case Comprehensive Cancer Center, both of which are affiliated with Case Western Reserve University in Cleveland.
Patients who did not experience any neurotoxic side effects might be distinguished from those who did so based on their NfL baseline levels. To see whether a bigger sample size will enable them to identify patients at risk of mild, moderate, or severe problems, the researchers intend to continue examining data from more patients.
The complications can range greatly from headaches, seizures, strokes, and brain swelling to difficulties concentrating, memory issues, disorientation, difficulty reading, and headaches. High-dose steroids and occasionally immune-modulating therapies that aim to lessen inflammation are the main ways that doctors treat these problems.
Since these therapies might, regrettably, impair the anti-cancer effect of the CAR-T cells, doctors would prefer to avoid using them whenever possible, thus it is very helpful to know who is at risk of the most harmful side effects.
Another puzzle is that even as some patients experience neurotoxic side effects and then recover from them, the elevated NfL levels are already present and largely stable. This implies that while NfL levels do not necessarily represent what is happening to cause the patients’ difficulties, they do indicate that something is wrong.
We’re just seeing the tip of the iceberg in terms of the actual disease process, and that’s where many of our future studies are going. We’re trying to get a better sense of what is causing these changes to begin with. And in later stages, even after symptoms have resolved, we still see these elevated NfL levels.”
Omar H. Butt, MD, PhD, Study Lead Author and Instructor, Medicine, Washington University School of Medicine in St. Louis
“We have a study ongoing at Siteman to see if, in fact, these patients continue to have subtle symptoms in terms of cognitive changes or deficits that persist long term,” remarked co-senior author Armin Ghobadi, MD, an associate professor of medicine and clinical director of the Center for Gene and Cellular Immunotherapy at Washington University School of Medicine and Siteman Cancer Center.
Source:
Journal reference:
Butt, O. H., et al. (2022) Assessment of Pretreatment and Posttreatment Evolution of Neurofilament Light Chain Levels in Patients Who Develop Immune Effector Cell–Associated Neurotoxicity Syndrome. JAMA Oncology. doi.org/10.1001/jamaoncol.2022.3738.