Prof. Kiavash Movahedi (VUB, VIB) headed a group that outlined how the immune system responds to infections entering the brain. The results offer new information on host-pathogen interactions as well as the long-term effects of brain infections.
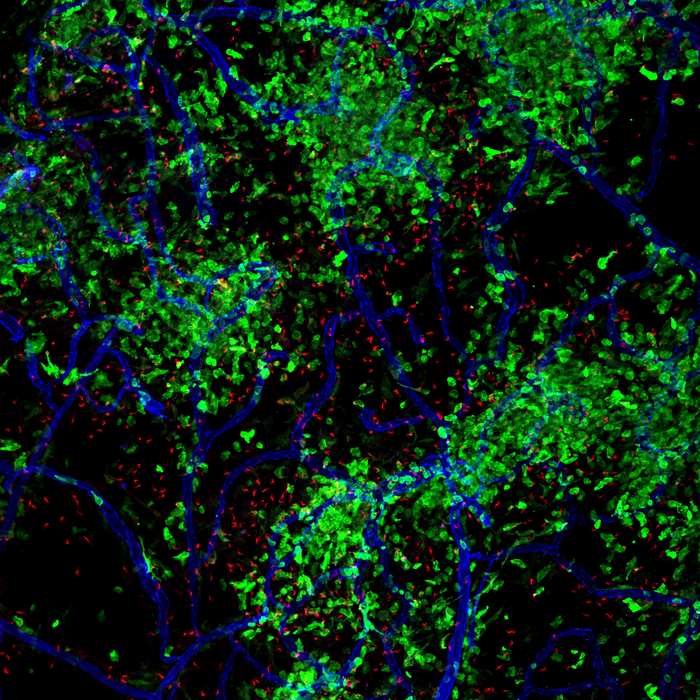 Parasites and macrophages in the meninges. Image Credit: Kiavash Movahedi.
Parasites and macrophages in the meninges. Image Credit: Kiavash Movahedi.
The observations, published in the prestigious journal Immunity, demonstrate how distinct kinds of immune cells participate in the defense against brain infections. The investigators were able to demonstrate that brain-resident macrophages, a type of white blood cell that already exists in the healthy brain, form the first line of defense.
These macrophages then attract a huge number of blood-derived macrophages, which aid in disease control. When the infection is cleared, these “recruited macrophages” go just as swiftly.
The study shows the remarkable ability of the brain’s immune landscape to quickly return to its normal state. But we could also observe how certain cells remained changed for a long time after healing, having a kind of ‘memory’ of the infection.”
Kiavash Movahedi, Professor, Vrije Universiteit Brussel
Kiavash Movahedi adds, “This suggests that during a lifetime, when we can suffer from numerous infections—think of the Covid-19 pandemic for example—the functionality of tissue macrophages can change. Do such earlier infections in the brain affect the likelihood of developing other neurological disorders, such as multiple sclerosis or dementia, for example? This will undoubtedly become a future hot topic in the research community.”
The brain and its defense against infections
Every process in the body is managed by the brain, which serves as a central command post. Therefore, it is crucial that the brain has a defense mechanism against disease. Complex barriers that prevent access to the brain help achieve this in part. As an additional line of defense, immune cells exist.
Some viruses nevertheless manage to get through these many layers of defense, which can cause deadly diseases. However, patients may experience neurological issues for years to come even if the disease is subsequently properly managed and the pathogens are cleared. Therefore, it is crucial to comprehend the dynamics of the host–pathogen relationship and its long-term effects.
The research
The research group led by Prof. Movahedi investigated brain-invading Trypanosoma brucei infections. These sub-Saharan African single-celled parasites have the potential to induce fatal neuropathology.
Although the presence of these parasites in the brain has long been known, nothing is known about how they enter the brain or how the host reacts to them. The group examined the infection in mice since they share with people a strong susceptibility to the disease.
Researchers discovered that the parasites first enter the meninges and choroid plexus, which are border tissues of the brain, before moving on to the fluid-filled cavities and the neuronal tissue. The scientists also meticulously mapped the immune system’s response using a number of cutting-edge technologies.
Macrophages play a significant role. They serve as the initial line of defense, sending signals throughout the body to draw blood-derived immune cells to the brain. Although the majority of these “newly recruited” immune cells are macrophages, they differ significantly from their resident counterparts.
Our results place macrophages at the center during pathogen invasion in the brain, and show how local and recruited macrophages play different roles during infection. For example, immune cells from the blood show higher expression of antimicrobial proteins. This suggests to us that they are well able to eliminate parasites.”
Karen De Vlaminck, Study First Author and PhD Student, Vrije Universiteit Brussel
The researchers subsequently examined what happened to all of these immune cells once the disease was effectively treated.
We were amazed at how fast the blood-recruited macrophages were removed from the brain as soon as the parasites were eliminated. This highlights how important it is for the brain to quickly return to its normal state once an infection has been dealt with.”
Kiavash Movahedi, Professor, Vrije Universiteit Brussel
Brain memory
The researchers discovered that resident macrophages in the brain’s border regions stayed activated for months after the parasites were eliminated, implying that they retained some type of “memory” of the infection. Investigations in other tissues have already shown that infection-induced memory can change macrophages’ capacity to respond to future infections.
De Vlaminck concludes, “However, this need not be as scary as it sounds. As we begin to understand the long-term impact of infections on the brain, research can start to focus on finding new therapies to address and reverse potential infection-induced dysfunctions.”
Source:
Journal reference:
De Vlaminck, K., et al. (2022) Differential plasticity and fate of brain-resident and recruited macrophages during the onset and resolution of neuroinflammation. Immunity. doi.org/10.1016/j.immuni.2022.09.005.