Hemophilia A is the most frequent severe variant of hemophilia. It nearly mostly affects men. The condition is frequently treatable, although not for all patients. A study at the University of Bonn has now highlighted a critical mechanism required for the therapy to be efficient.
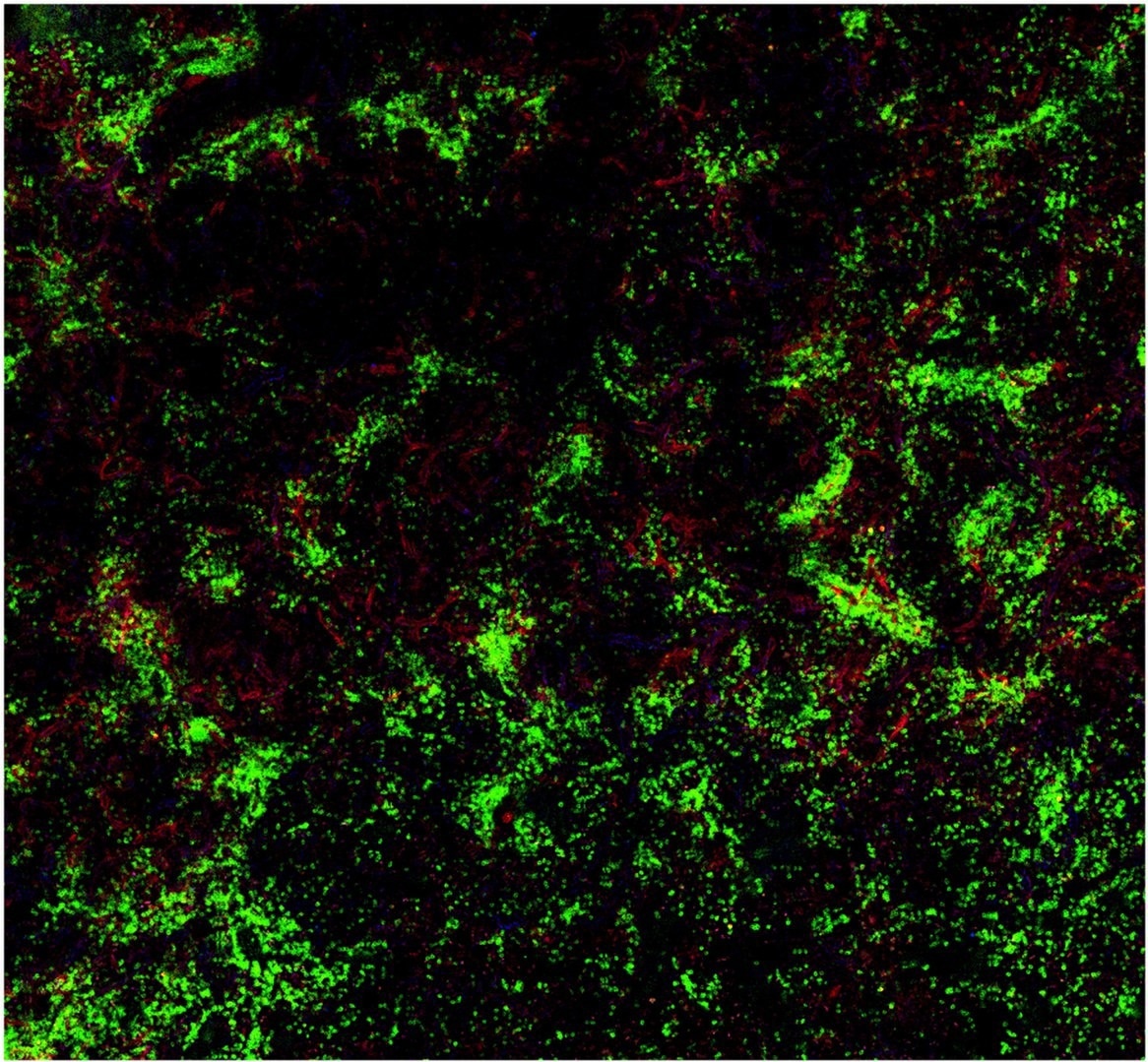 Tissue sample from the spleen of a mouse: The B cells (green) interact with factor VIII (red). Image Credit: © AG Becker-Gotot/University Hospital Bonn
Tissue sample from the spleen of a mouse: The B cells (green) interact with factor VIII (red). Image Credit: © AG Becker-Gotot/University Hospital Bonn
The findings could aid in better tailoring treatment to patients. They have already been published online in an initial version; the final version will be published soon in the Journal of Clinical Investigation.
Patients with hemophilia A have a mutation in factor VIII, a protein essential for blood clotting. As a result, most patients are treated with an intravenous injection of the functioning clotting factor every few days.
However, the immune system frequently perceives the injected substance as alien to the body and assaults it, especially at the beginning of treatment. This is the most significant complication of hemophilia treatment since factor VIII is no longer able to function.
Immune tolerance therapy, which was also established at the University Hospital Bonn (UKB) over 40 years ago, is typically helpful in these circumstances. This entails giving the hemophiliacs a high dose of factor VIII on a regular basis for several months. As a result, the immune system becomes accustomed to and tolerates the injected protein. The immunological mechanisms at work are unknown.
However, this doesn’t always work. In about 30 percent of patients, tolerance induction does not lead to success. So your body’s own defenses continue to attack and destroy the factor VIII protein, which means that factor VIII cannot be used for treatment. We wanted to know the reason for this.”
Dr Johannes Oldenburg, Professor and Director, Institute for Experimental Haematology and Transfusion Medicine, University Hospital Bonn
To achieve this, the scientists examined B cells and regulatory T cells, two immune system cell types. B cells identify foreign molecules in the body and generate antibodies against them, which inhibit the molecule’s function. This means that factor VIII is no longer useful in the treatment of hemophilia.
Brake in the immune system
Regulatory T cells keep an immune response from becoming too powerful or lasting too long. Scientists have discovered a novel sort of them that can work directly against specific B cells rather than acting broadly against all immune responses.
We were able to show that immunotolerance therapy results in the generation of regulatory T cells that exclusively induce B cells against factor VIII to commit suicide. These T cells have a sensor that allows them to recognize and attach to the corresponding B cells. In addition, they have the ability to push the self-destruct button on the surface of B cells.”
Dr Janine Becker-Gotot, Institute of Molecular Medicine and Experimental Immunology, University Hospital Bonn
A molecule known as PD-1 serves as this button. It does this by turning on a program in the B cell that eventually kills it. This button is present on every functioning B cell.
“Our experiments enabled us for the first time to detect regulatory T cells that can activate this self-destruct button only in very specific B cells, in order to specifically prevent unwanted immune responses,” detailed IMMEI Director Prof. Dr Christian Kurts.
Immune tolerance therapy can more easily induce the death of B cells against factor VIII the more PD-1 buttons they have on their surface.
The amount of PD-1 varies from person to person. If it's very low to begin with, there's a good chance that many inhibitor-producing B cells will survive and continue to neutralize the injected factor VIII.”
Dr Janine Becker-Gotot, Institute of Molecular Medicine and Experimental Immunology, University Hospital Bonn
Test to show in whom immunotolerance therapy is useful
Importantly, when B cells interact with regulatory T cells, they also create more PD-1.
The investigators note, “We can now test how strong this reaction is. If PD-1 levels go up shortly after starting immune tolerance therapy and then stay up, that's a clear sign that the treatment is going to be successful.”
The group is presently working on a blood test that will be able to determine whether or not immunological tolerance therapy is functioning in patients over the prolonged course of treatment.
Prof. Kurts, who is a member of the Transdisciplinary Research Area “Life & Health” at the University of Bonn and, like Dr Becker-Gotot and Prof. Oldenburg, a member of the Cluster of Excellence ImmunoSensation concludes, “Our findings have great basic scientific value. And not just for hemophilia, but also for other congenital disorders where missing proteins are replaced therapeutically. In the long term, they could also be used to develop new treatments.”
Source:
Journal reference:
Becker-Gotot, J., et al. (2022) Immune tolerance against infused FVIII in hemophilia A is mediated by PD-L1+ regulatory T cells. The Journal of Clinical Investigation. doi.org/10.1172/jci159925.