Cells competing for a place in a germinal center confront a tough admissions process. Germinal centers, which form following exposure to a pathogen or vaccine, serve as a kind of immune system training academy, assisting B cells in refining their response to the threat. Only B cells with the strongest affinity for the pathogen or vaccine are allowed to enter these structures, where they undergo waves of mutations to make progressively stronger antibodies.
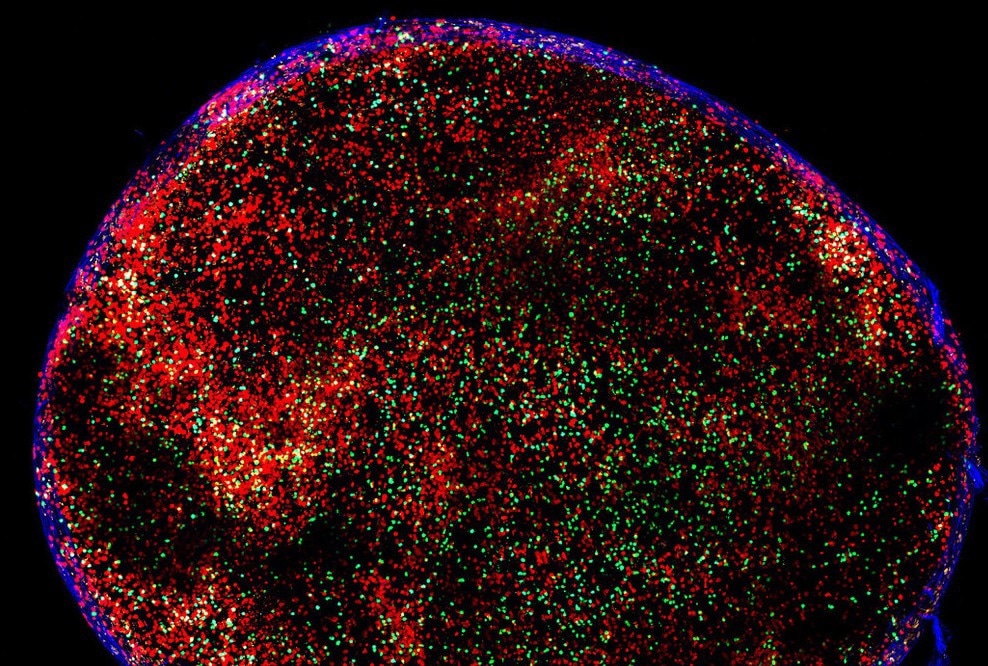 A mouse lymph node, containing B cells and T cells. Image Credit: The Rockefeller University
A mouse lymph node, containing B cells and T cells. Image Credit: The Rockefeller University
However, one peculiarity of this process has long confused researchers: germinal centers appear to vary their admission criteria over time. In the later stages of a germinal center’s existence, B cells with little or no affinity for the virus penetrate the once-exclusive site, eventually accounting for up to 30% of its graduates.
A new study published in Cell discusses this phenomenon in depth and implies that high-affinity B cells—the exact ones that sideline inferior B cells in the early stages—trigger this about-face in late-stage germinal centers. The findings give new information on how the immune system responds to infections like COVID and HIV.
Germinal centers are open structures that continuously receive B cells. As time goes on, the threshold for joining is lowered, and this leads to a more diverse set of responder cells.”
Michel C. Nussenzweig, Zanvil A. Cohn and Ralph M. Steinman Professor, The Rockefeller University
Inside a germinal center
Nussenzweig and coworkers tracked B cells in germinal centers in mice for the study. They initially proved that B cells reach early-stage germinal centers based on their capability to attach to a vaccine antigen. Due to the scarcity of antigens in the area, high-affinity B cells (those with receptors that are particularly good at binding the antigen) nab an antigen and are duly allowed into the germinal center. Lower affinity B cells are left to bumble around on the outside.
So, how do low-affinity antibodies access the late-stage germinal center? Further research revealed that in the late-stage germinal center, elite B cells begin producing antibodies that attach to dendritic cells presenting antigens.
A dense forest of antigen-antibody complexes begins to obstruct the area, causing a molecular traffic jam. As a result, the once scarce antigen is now abundantly available. Low-affinity B cells attach to whatever antigen is available and use it to enter the germinal center.
This suggests that the same high-affinity B cells that push low-affinity B cells out of the germinal center early on set in motion the process by which those inferior cells are ultimately admitted.
Our paper not only outlines and documents this phenomenon. It shows that the mechanism by which it happens is antibody-dependent.”
Michel C. Nussenzweig, Zanvil A. Cohn and Ralph M. Steinman Professor, The Rockefeller University
A double-edged sword
Introducing naive B cells into the germinal center fulfills one of the immune system's primary goals.
Diversity is a key feature of immunity. The immune system as a whole does many things to maximize diversity, and here germinal centers are striving for a diverse immune response by lowering the threshold and letting more cells join.”
Michel C. Nussenzweig, Zanvil A. Cohn and Ralph M. Steinman Professor, The Rockefeller University
When naive B cells enter the late-stage germinal center, they have far less time to mutate and will certainly differ from the elite B cells that were present all along. Depending on the virus in question, this kind of variation in the range of immune cells that come into contact with the pathogen can either help or hinder it. “It can be a very positive or very negative thing,” states Nussenzweig.
Consider SARS-CoV-2, a virus having multiple antigen bits (called epitopes) that antibodies can utilize to recognize and attach to the virus. After leaving the germinal center, naive B cells create antibodies that attach to multiple epitopes, each attacking the virus from a different angle. If the virus mutates, rendering one antibody ineffective or obsolete, the others can still offer coverage.
Nussenzweig adds, “Diversity gives you more targets, and you can make antibodies to other parts of the molecule. For SARS viruses, it’s terrific, and in part responsible for our ability to fight off variants when we do get infected.”
This is not the case with HIV, a virus with very few epitopes. According to Nussenzweig and coworkers’ latest work, if the body recognizes an excess of minimally effective antibodies, it shuts off the creation of an entire line of antibodies. In this case, a broad response raises the risk of low-affinity antibodies attaching one of HIV’s only epitopes poorly, causing the body to turn off a large component of the immune response. Similar antibodies that might have performed better may never be allowed to form.
“For HIV, it gets in the way of an effective vaccine,” says Nussenzweig.
The researchers believe that their findings will help guide future vaccine development efforts while also expanding immunologists’ understanding of how the body responds to disease.
Source:
Journal reference:
Hägglöf, T., et al. (2023) Continuous germinal center invasion contributes to the diversity of the immune response. Cell. doi.org/10.1016/j.cell.2022.11.032.