An investigation has been performed by scientists as to how disease-causing fungi become resistant to antifungal drugs to help avoid possibly detrimental impacts of the growing resistance harmful microbes are developing to drugs.
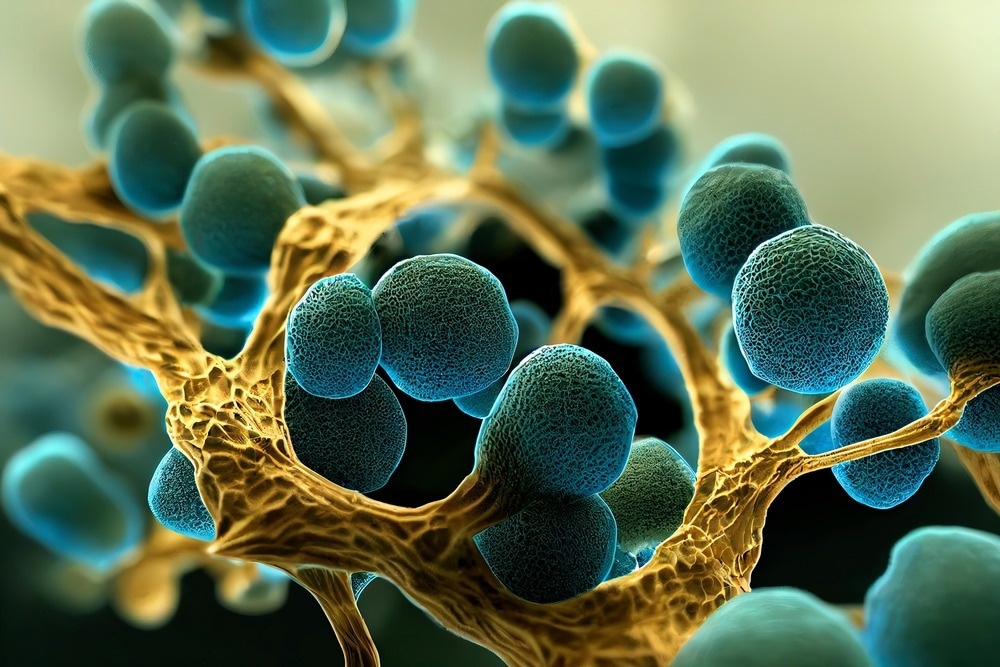
Image Credit: Vikks/Shutterstock.com
Antimicrobial drugs are fundamental for us to live healthy lives.”
Daniel Charlebois, Study Co-Author and Assistant Professor, Department of Physics, Adjunct Professor, Department of Biological Sciences, University of Alberta
When microbes affecting the body create permanent resistance to a drug, that drug becomes futile or less effective in battling the infection that it has been designed to target.
By adopting two ways, cells tend to develop resistance to antimicrobial drugs, Charlebois describes: genetically or non-genetically.
Genetic resistance is known to be permanent and is also passed down to offspring. It is only in the past decade or so that scientists have started digging into non-genetic resistance. There is an occurrence of a lost piece of the puzzle when cells are shifting between these two resistant states—and that is what Charlebois hopes to clarify with his work.
Gaining better insight into the shift between the two kinds of resistance is significant to identify methods to avoid cells from mutating and progressing to develop genetic resistance.
People tend to be experts in one or the other forms of resistance, and it’s only now that we’re really starting to look at this interplay.”
Daniel Charlebois, Study Co-Author and Assistant Professor, Department of Physics, Adjunct Professor, Department of Biological Sciences, University of Alberta
Charlebois added, “Trying to understand how these non-genetic mechanisms influence evolution is really interesting for drug resistance, which is an evolutionary process.”
The study performed by Charlebois displayed that when there is an existence of both genetically and non-genetically resistant cells, it takes a prolonged period for the population of cells to become completely genetically resistant since the two kinds of cells are competing for resources like space and nutrients.
It takes longer for those genetically resistant mutants to spread and become more than 95 percent of the population.”
Daniel Charlebois, Study Co-Author and Assistant Professor, Department of Physics, Adjunct Professor, Department of Biological Sciences, University of Alberta
As soon as a cell mutates to turn genetically resistant, it remains that way. But a non-genetically resistant cell can become a so-called “susceptible cell,” implying it will die or quit growing in the existence of the drug. It is possible to treat an infection with the resistance removed.
A population model was created by Charlebois and physics master’s student Joshua Guthrie to analyze the various subpopulations of resistant cells.
Charlebois stated, “We are considering the population dynamics, whereas before it was just considered one population [of resistant cells].”
A code was developed by Guthrie and simulation work was performed to simplify the process and narrow down numerous experiments that would have to be done in the laboratory. The research’s modeling portion offered main information, like when the first mutation occurs in a cell.
“That might inform when you should add or change drugs during treatment,” stated Charlebois.
A greater understanding of the interplay between the various resistance mechanisms could provide physicians with vital information regarding what kind of drugs to administer and what treatment schedule would be most beneficial.
For instance, alternating drugs to utilize trade-offs in vulnerable, non-genetically resistant, and resistant subpopulations during treatment might assist in keeping the genetically resistant subpopulation at bay for a long time. This could inform treatment options like sequential or combination therapies, states Charlebois.
Charlebois stated, “You’re dealing with a population of interacting entities, different types of potential drug resistance. Thinking of ways to exploit that is not something that is typically considered when you’re developing treatments.”
Source:
Journal reference:
Guthrie, J. D., et al. (2022) Non-genetic resistance facilitates survival while hindering the evolution of drug resistance due to intraspecific competition. Physical Biology. doi.org/10.1088/1478-3975/ac8c17