Until now, the use of models to study the barrier that differentiates the circulatory and nervous systems has been either limited or extremely complex. ETH Zurich researchers have created a more accurate model that can also be used to effectively investigate new treatments for brain tumors.
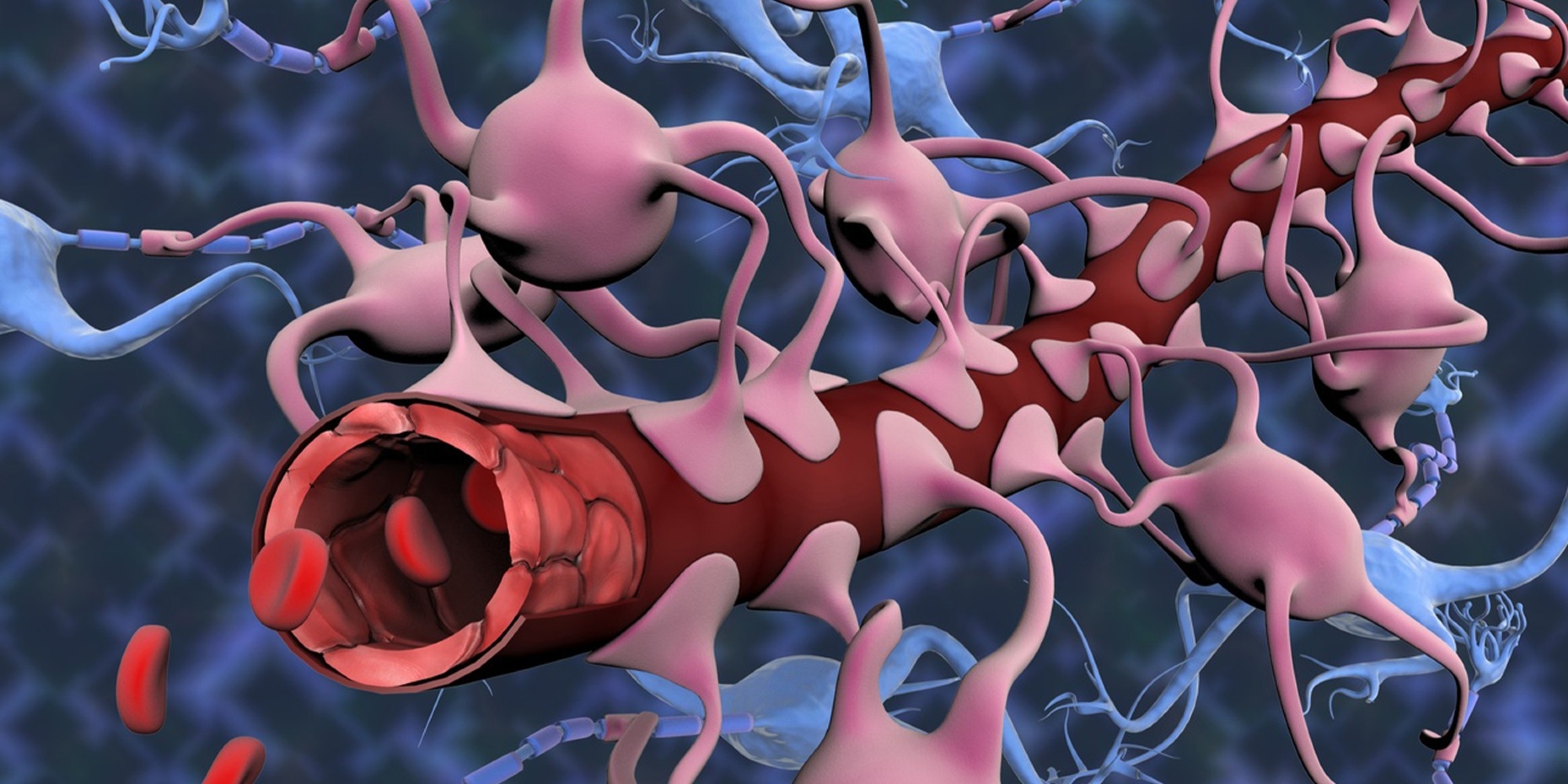 In order to better understand how the blood-brain barrier protects the central nervous system from harmful substances in the bloodstream, ETH researchers have developed a new in-vitro model. Image Credit: Gunilla Elam/Science Photo Library.
In order to better understand how the blood-brain barrier protects the central nervous system from harmful substances in the bloodstream, ETH researchers have developed a new in-vitro model. Image Credit: Gunilla Elam/Science Photo Library.
Mario Modena is a postdoc at ETH Zurich’s Bio Engineering Laboratory. He would tell an 11-year-old, “This wall is important because it stops the bad guys from getting into the brain,” about his research on the blood-brain barrier, which protects the central nervous system from dangerous substances in the bloodstream.
He claims that if the brain is damaged or sick, holes in the wall can appear. Such holes can sometimes be beneficial, such as when supplying the brain with desperately needed medicine. “So what we are trying to understand is how to maintain this wall, break through it and repair it again,” Modena adds.
This barrier is also significant from a medical standpoint since many central nervous system diseases are related to blood-brain barrier damage. Researchers frequently perform experiments on live animals to learn how this barrier works.
Aside from being relatively expensive, such experiments may only provide a partial picture of what is going on in the human body. Furthermore, some critics question the fundamental validity of animal testing. An alternative would be to base experiments on laboratory-cultivated human cells.
Cell-cell communication largely overlooked
The issue with several in-vitro models is that they use blood-vessel-wall cells (endothelial cells) to replicate the blood-brain barrier in a comparatively simplified manner. This method fails to represent the complex structure of the human system and ignores, for example, communication between cell types.
In addition, most of these models are static. In other words, the cells are suspended in a non-moving suspension, implying that fluid flow or shear stress experienced by the cells in the body is not considered.
There are also interactive in-vitro models that simulate flow conditions in the body, but the pumps required make the experimental setup complicated. Along with all of these hurdles, there is the issue of measurement: taking high-resolution images of structural changes to the blood-brain barrier in real time while also assessing the barrier’s electrical resistance, both of which reflect barrier compactness and tightness, is nearly impossible.
Killing several birds with one stone
If these hurdles were birds, Modena’s platform would be the stone that tries to kill them all. Modena and his co-workers invested three and a half years in creating the open-microfluidic 3D blood-brain barrier model under Andreas Hierlemann’s supervision.
To replicate the barrier, the researchers merged cell types found naturally in the blood-brain barrier—microvascular endothelial cells, human astrocytes, and human pericytes—on a single platform.
This strategy allowed us to almost fully replicate the 3D cell structure found in the human body. But what’s really exceptional is that we can measure the barrier’s permeability while simultaneously mapping morphological changes to the barrier by means of high-resolution time-lapse microscopy.”
Mario Modena, Bio Engineering Laboratory, ETH Zurich
To enable this double act, the scientists deposited completely transparent electrodes on both sides of the cell barrier to quantify its permeability, which is mirrored in the electrical resistance across the cell barrier. Transparent electrodes have a considerable advantage over other electrode types, such as metal films or wire structures, which can intrude with optical detection and high-resolution microscopy.
“Without increasing the complexity”
The scientists have created a microfluidic platform with fluid reservoirs at both ends of a seesaw to mimic how fluid flows in the body. Gravity then stimulated the flow, which produced shear force on the cells. Hierlemann explains the advantage of this configuration: “Since we are not using any pumps, we can experiment with multiple model systems simultaneously, for instance in an incubator, without increasing the setup complexity.”
The scientists presented and evaluated their new in vitro blood–brain barrier model in a study published recently in the journal Advanced Science. Researchers exposed the barrier to oxygen-glucose deprivation, as occurs during a stroke.
These experiments allowed us to trigger rapid changes in the barrier and demonstrate the platform’s potential.”
Mario Modena, Bio Engineering Laboratory, ETH Zurich
Pharma company already showing an interest
Modena and his co-workers were successful in accomplishing more than simply demonstrating that their new platform is capable of measuring. They also found that the electrical resistance of the barrier lowers even before it endures morphological changes that make it permeable.
“This finding could prove relevant for future research,” Modena says. The group also discovered that the barrier was more permeable in control experiments using a static in-vitro model than in the new dynamic setup.
It is clear that the shear force, generated by the gravity-driven flow, promotes the formation of a denser barrier layer, which confirms how important flow is for representative in-vitro models.”
Mario Modena, Bio Engineering Laboratory, ETH Zurich
Modena and Hierlemann strongly feel that their model will make it a lot easier to identify which molecules stabilize the barrier and to find compounds and methods for crossing it that could be used to treat brain tumors. However, Hierlemann believes that the model could influence future in-vitro research.
Hierlemann notes, “The advantage of our platform is that it is very easy to adapt to other endothelial cell models, where a combination of barrier-tightness measurements and high-resolution microscopy could pave the way to new research.” The industry has expressed interest in the new model. A pharmaceutical company has already reached out to the researchers.
Source:
Journal reference:
Wei, W., et al. (2023) 3D In Vitro Blood-Brain-Barrier Model for Investigating Barrier Insults. Advanced Science. doi.org/10.1002/advs.202205752.