The product of a gene expressed in most cancers, including the most prevalent type of head and neck cancer, has been linked to elevated levels of white blood cells that produce antibodies inside tumors, according to researchers at the University of California San Diego School of Medicine and UC San Diego Moores Cancer Center.
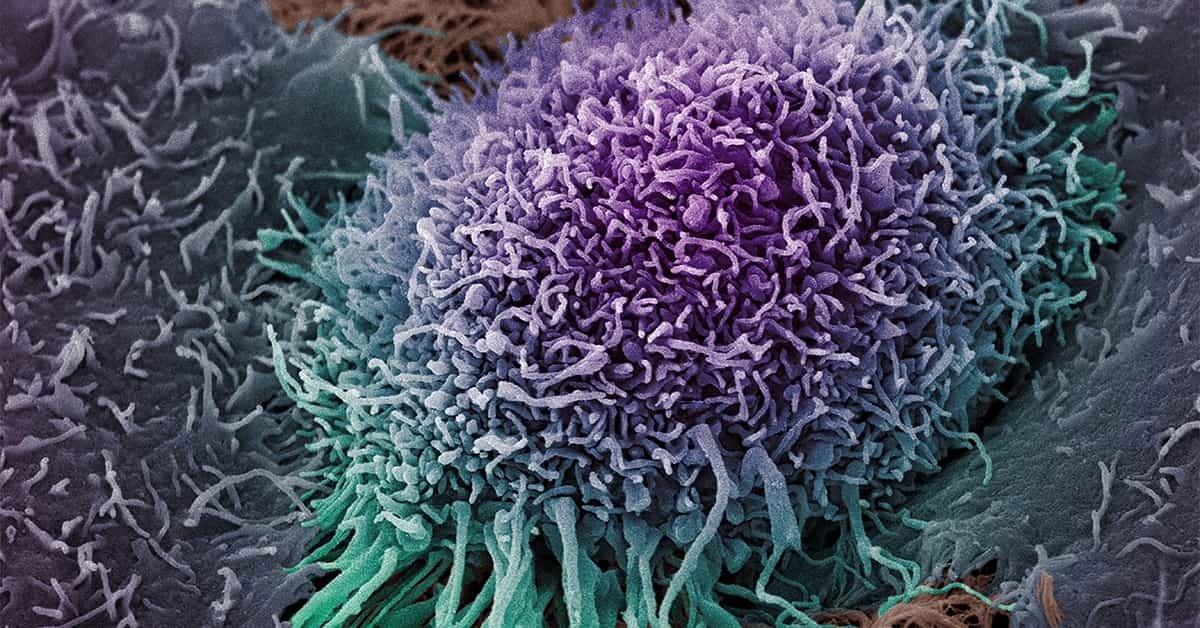 A colorized scanning electron micrograph depicts a single human oral squamous carcinoma cell, the most common form of head and neck cancer. Image Credit: Wellcome Collection
A colorized scanning electron micrograph depicts a single human oral squamous carcinoma cell, the most common form of head and neck cancer. Image Credit: Wellcome Collection
The study, which was published in PNAS Nexus on March 10th, 2023, indicates a prospective new target and approach for cancer immunotherapies, which have so far shown varying degrees of success in treating certain head and neck cancers.
Around 85% of tumor cells generate a large amount of the antigen telomerase reverse transcriptase (TERT). Toxins or other substances are considered antigens since they cause the immune system to react negatively to them. With TERT in cancer patients, this is certainly relevant.
Yet, it is unclear how TERT expression affects the regulation of adaptive immunity in tumors. RNA sequencing data from The Cancer Genome Atlas was used in the current study by Maurizio Zanetti, MD., co-senior study author, professor of medicine at the UC San Diego School of Medicine, and head of the Laboratory of Immunology at Moores Cancer Center.
Our data emerged through targeted computational reanalysis of The Cancer Genome Atlas, a valuable public tumor sequencing dataset, guided by core principles of immunology.”
Hannah Carter, Ph.D, Study Co-Senior Author and Associate Professor, School of Medicine, University of California San Diego
Zanetti, Carter, and their colleagues investigated possible relationships between TERT expression and B and T cells infiltrating the tumor microenvironment in 11 solid tumor types.
B cells are immune response cells that create antibodies against antigens such as bacteria, viruses, and toxins. T cells are immune cells that attack and destroy cells in the body that have been infected with antigens or malignant. Yet, B cells also deliver antigens to T cells, activating them in the process.
The researchers discovered a link between TERT expression and B and T cells in four cancer types, with the strongest link reported in head and neck squamous cell carcinoma, a condition that originates in the mucous membranes of the mouth, nose, and throat.
They discovered that patients in whom this correlation was discovered had better clinical results. According to Zanetti, the findings point to the de novo creation of lymphoid structures within tumors by B and T lymphocytes, with TERT serving as a possible connecting antigen.
HNSCC (head and neck squamous cell carcinoma) is the sixth most prevalent type of cancer. It is responsible for 90% of all head and neck cancers. Long-term cigarette use, alcohol intake, and infection with high-risk strains of the human papillomavirus are the leading causes of the disease.
Each year, roughly 66,000 new cases of head and neck cancer are diagnosed in the United States, with 15,000 fatalities. The death rate for HNSCC is high. About 50 to 60% of patients die within a year after diagnosis, with a five-year survival rate of 50% (patients living five years after diagnosis).
Chemotherapy, radiation, and immune checkpoint therapy are used to treat HNSCC tumors that cannot be removed surgically, albeit only a tiny percentage of patients benefit from the immune checkpoint therapy.
According to Zanetti, the new findings suggest potentially innovative approaches to treating HNSCC, particularly in individuals at higher risk of poor outcomes.
Cancer immunotherapy is about treating a patient by leveraging their own immune system to fight the malignancy. Ideally, one should reinforce mechanisms already in place in patients.”
Maurizio Zanetti, MD., Study Co-Senior Author and Professor, Medicine, School of Medicine, University of California San Diego
He added, “The current emphasis is on neoantigens (proteins that form on cancer cells when certain mutations occur in tumor DNA) and immune checkpoint inhibitors (drugs such as monoclonal antibodies) that target and block actions that help shield cancer cells from attack by T cells.”
“But these therapies only partially effective and in some types of cancer only. Our findings provide evidence that high TERT expression is a key signal that generates high levels of B and T cells intra-tumor, suggesting a new way to develop intra-tumor immunotherapies to reinforce anti-tumor immunity already in place,” Zanetti concluded.
Source:
Journal reference:
Xian, S., et al. (2023). Transcriptional analysis links B cells and TERT expression to favorable prognosis in head and neck cancer. PNAS Nexus. doi.org/10.1093/pnasnexus/pgad046