A study discovered that the magnitude and quality of a key immune cell’s response to two doses of the Pfizer-BioNTech COVID-19 vaccine were significantly lower in individuals with earlier SARS-CoV-2 infection compared to individuals without previous infection.
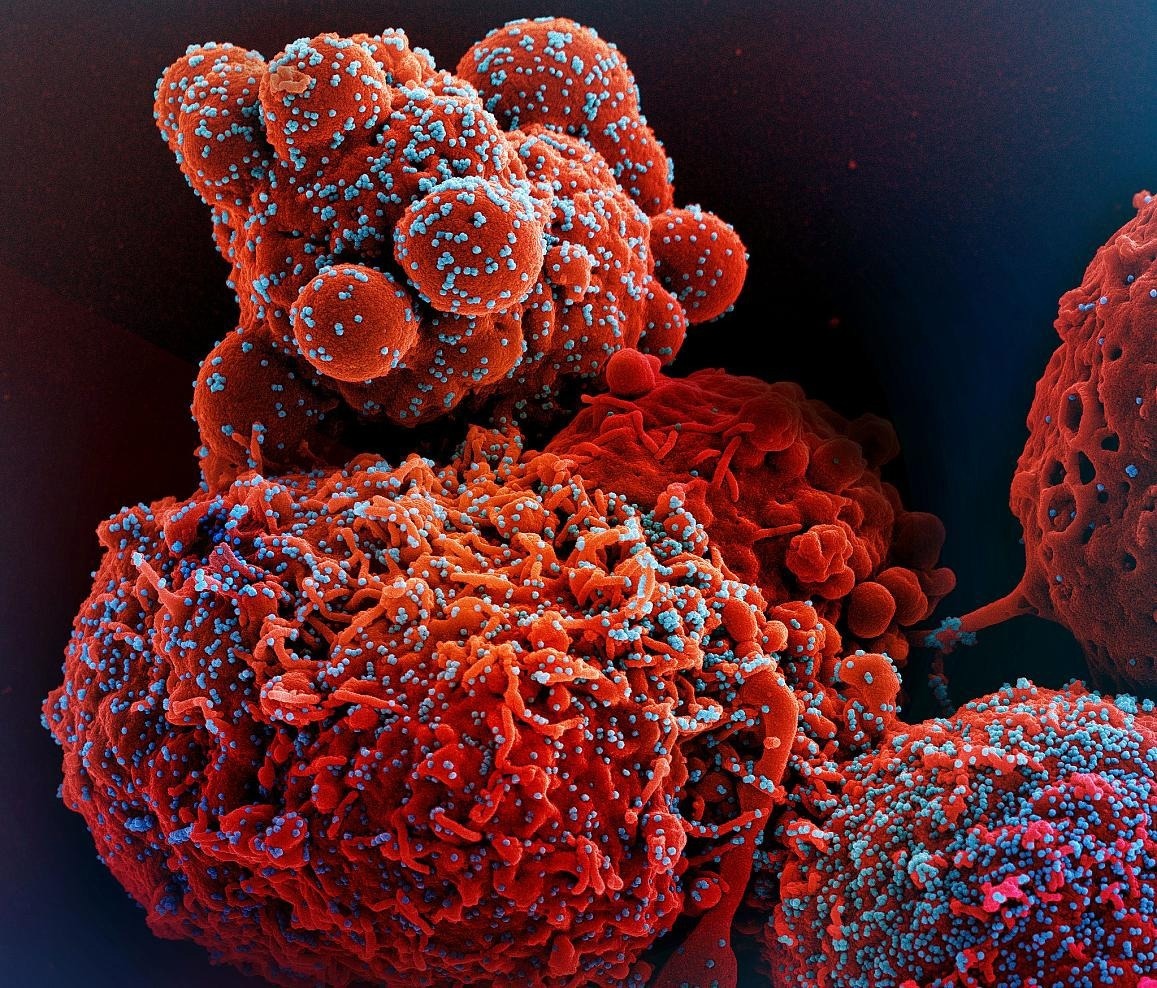 Colorized scanning electron micrograph of a cell (red) infected with the Omicron strain of SARS-CoV-2 virus particles (blue), isolated from a patient sample. Image Credit: National Institute of Allergy and Infectious Diseases.
Colorized scanning electron micrograph of a cell (red) infected with the Omicron strain of SARS-CoV-2 virus particles (blue), isolated from a patient sample. Image Credit: National Institute of Allergy and Infectious Diseases.
Furthermore, the extent of this key immune cell that identifies the SARS-CoV-2 spike protein in unvaccinated individuals with COVID-19 was significantly lower than in vaccinated individuals who had never been infected.
Notably, people who recover from SARS-CoV-2 infection and then get vaccinated are better protected than unvaccinated people. These observations, which indicate that the virus interferes with a vital immune-cell response, were published today in the journal Immunity.
The research was funded in part by the National Institute of Allergy and Infectious Diseases (NIAID), which is part of the National Institutes of Health, and was guided by Mark M. Davis, PhD.
Dr Davis is the Director of Stanford University School of Medicine’s Stanford Institute for Immunity, Transplantation, and Infection and a Professor of microbiology and immunology. In addition, he is a Howard Hughes Medical Institute Investigator.
Dr Davis and co-workers created a highly sensitive tool to study how immune cells known as CD4+ and CD8+ T cells respond to SARS-CoV-2 infection and vaccination. These cells help to prevent COVID-19 by coordinating the immune system’s response to the virus and killing infected cells.
The tool was created to detect T cells that aim any of the dozens of distinct regions on the virus’ spike protein, and other viral regions. Parts of the SARS-CoV-2 spike protein are used in the Pfizer-BioNTech vaccine to evoke an immune response without causing infection.
The researchers looked at CD4+ and CD8+ T-cell responses in blood samples from three different groups of volunteers. One group had never had SARS-CoV-2 infection and obtained two doses of the Pfizer-BioNTech COVID-19 vaccine.
The second group had been infected with SARS-CoV-2 and got two doses of the vaccine. The third group had COVID-19 and had not been vaccinated.
The vaccine induced robust CD4+ and CD8+ T-cell responses to the virus’ spike protein in individuals who had never been infected with SARS-CoV-2, according to the researchers. Furthermore, these T cells produced a variety of cell-signaling molecules known as cytokines, which attract other immune cells, including antibody-producing B cells, to combat pathogens.
Individuals who had been infected with SARS-CoV-2 prior to vaccination, on the other hand, produced significantly fewer spike-specific CD8+ T cells—and with less functionality—than vaccinated people who had never been infected. Furthermore, unvaccinated people with COVID-19 had significantly lower levels of spike-specific CD8+ T cells than vaccinated people who had never been infected.
Taken together, the results indicate that SARS-CoV-2 infection impacts the CD8+ T cell response, an effect similar to that observed in previous studies demonstrating long-term immune system damage after infection with viruses like hepatitis C or HIV.
According to the researchers, the latest findings emphasize the need to develop vaccination strategies that particularly enhance antiviral CD8+ T cell responses in people who have previously been infected with SARS-CoV-2.
Source:
Journal reference:
Gao, F., et al. (2023). Robust T cell responses to Pfizer/BioNTech vaccine compared to infection and evidence of attenuated peripheral CD8+ T cell responses due to COVID-19. Immunity. doi.org/10.1016/j.immuni.2023.03.005.