Human pluripotent stem cells were effectively transformed into purified pituitary cells, which aggregated into hormone-secreting organoids. The transplantation of these 3D pituitaries into mice with hypopituitarism resulted in long-term improvements in levels of adrenocorticotropic hormone (ACTH), which is generally produced and secreted by the pituitary gland.
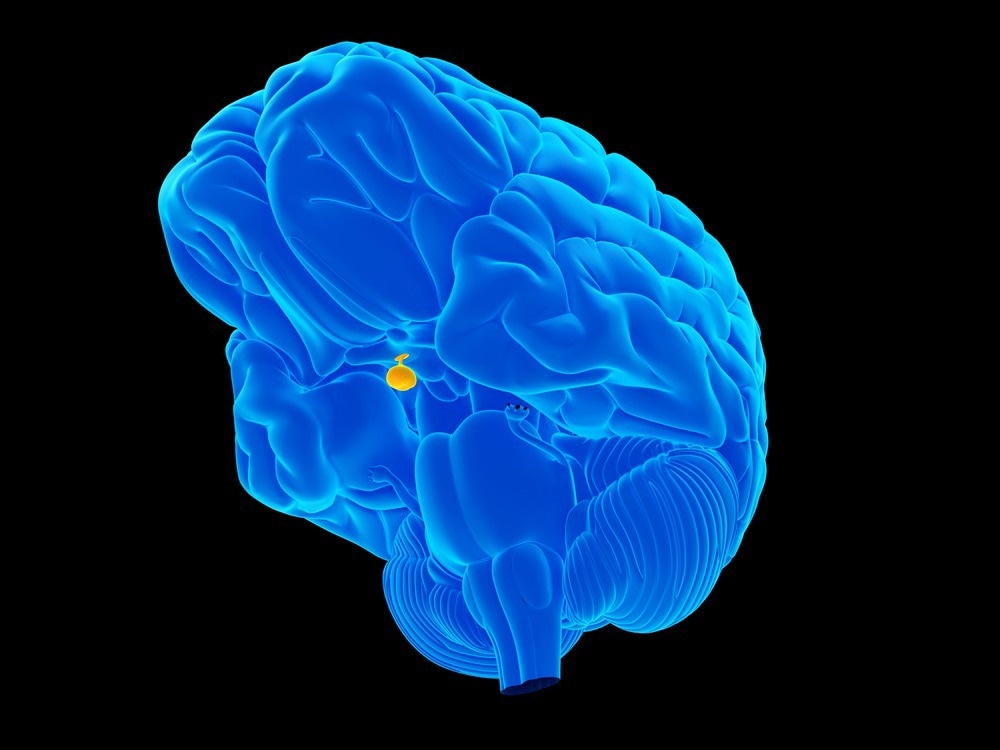
Image Credit: SciePro/Shutterstock.com
The study was published on June 8th, 2023, in the journal Stem Cell Reports.
This method of generating purified pituitary tissue opens new avenues of research for pituitary regenerative medicine.”
Hidetaka Suga, Study Author, Nagoya University
The pituitary gland controls hormones, which influence a variety of processes, including growth, metabolism, stress responses, and reproduction. Low blood pressure, reduced consciousness, electrolyte imbalance, growth abnormalities, and infertility can all occur from pituitary-gland dysfunction. There is currently no cure for hypopituitarism or the pituitary gland’s low release of hormones. As a result, this disorder requires lifelong hormone replacement.
Pituitary organoids are promising graft sources for transplantation for the treatment of hypopituitarism. The generation of stem cell-based human pituitary tissue that responds to the surrounding environment could lead to improvements in regenerative-medicine treatments for hypopituitarism.”
Hidetaka Suga, Study Author, Nagoya University
The researchers devised ways to produce and purify pituitary cells obtained from human pluripotent stem cells for clinical applications in the investigation. The purified pituitary cells clustered together to form pituitary spheres with a high capacity to produce ACTH. ACTH-producing cells were found in all pituitary-hypothalamic organoids.
When engrafted 3D pituitaries were transplanted into hypopituitarism mice, they survived for half a year, resulting in long-term improvement in ACTH levels and adequate ACTH responses. Corticotropin-releasing hormone, a peptide hormone involved in stress responses, was identified by the transplanted cells.
Negative feedback from the glucocorticoid dexamethasone overrode positive stimulation from corticotropin-releasing hormone in the transplanted 3D pituitaries, potentially lowering the adverse effects of ACTH replacement.
Since the 3D pituitaries receive steroid feedback via systemic circulation, the risk of Cushing’s disease—a condition in which the pituitary gland produces excessive ACTH—is low.
Our strategies open new avenues toward high-quality pituitary cell production suitable for pituitary regenerative medicine. For non-clinical or clinical studies, we will continue to develop manufacturing methods for clinical-grade cell lines, evaluate the efficacy of these lines in animals such as monkeys, and confirm the functionality of products after transplantation.”
Hidetaka Suga, Study Author, Nagoya University
Source:
Journal reference:
Taga, S., et al. (2023). Generation and purification of ACTH-secreting hPSC-derived pituitary cells for effective transplantation. Stem Cell Reports. doi.org/10.1016/j.stemcr.2023.05.002.