New research published in Nature Metabolism discovered the pathogenic mechanism driving mitochondrial enoyl reductase protein-associated neurodegeneration (MEPAN) syndrome, a rare pediatric neurodegenerative disease. Dr Hugo J. Bellen, distinguished service professor at Baylor College of Medicine and Chair of Neurogenetics at Texas Children’s Hospital’s Jan and Dan Duncan Neurological Research Institute (Duncan NRI), and Dr Debdeep Dutta, a postdoctoral associate in the Bellen group, conducted the study.
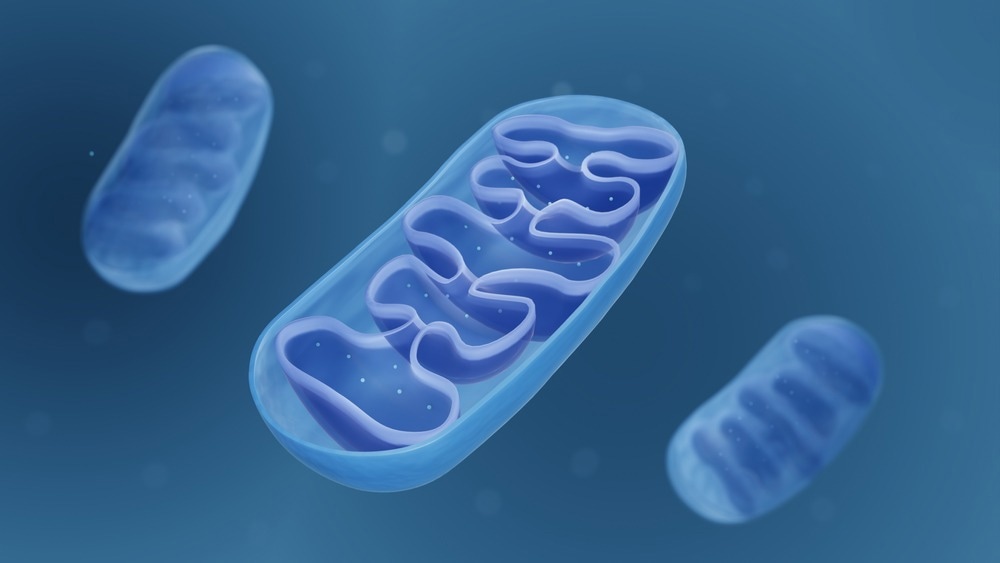
Image Credit: ART-ur/Shutterstock.com
The Duncan NRI team discovered that a high percentage of neurons die in people and animal models of this condition due to excessive ceramide buildup and faulty iron metabolism caused by changes in mitochondrial fatty acid production. It is the first to show a relationship between mitochondrial fatty acid production, iron and ceramide metabolism, and neurodegeneration.
Fatty acids are the primary building blocks of the body’s complex lipids. The bulk of fatty acids are generated in the cytoplasm, the gelatinous liquid that fills the majority of cells in most multicellular creatures, including humans. It was revealed in the late 1980s that a tiny proportion of fatty acids are also generated in the mitochondria, which serve as the cell's energy producers.
Mutations in the mitochondrial enoyl coA-reductase (MECR) gene were discovered to be the cause of MEPAN syndrome, a rare neurological disease characterized by progressive movement abnormalities such as dystonia, speech difficulties, and vision loss, finally leading to blindness.
The MECR gene produces an enzyme that catalyzes the last stage in mitochondrial fatty acid production, but nothing was known about how the interruption of this gene affects neuronal stability and function.
To decipher which biological processes and pathways go awry when the MECR gene is disrupted, we used CRISPR technology to delete this gene in fruit flies.”
Dr. Hugo J. Bellen, Chair of Neurogenetics, Jan and Dan Duncan Neurological Research Institute, Texas Children’s Hospital
They discovered that flies lacking both copies of the mecr gene did not survive, but the existence of one undamaged copy of the fly or human version of this gene was sufficient for survival. Only a tiny percentage of the flies expressing the mutant (disease-causing) version survived, demonstrating that the mortality was caused by the loss of MECR gene function.
Flies expressing the mutant variant of the fly mecr gene demonstrated increased age-related movement difficulties, decreased neuronal activity in retinal neurons, and other symptoms of neurodegeneration, similar to MEPAN patients.
Interestingly, we found that mitochondria in mecr mutants and fibroblast cells from MEPAN patients were structurally and functionally abnormal. Further, lipidomic and other analyses revealed that although the levels of the majority of phospholipids remained unaltered, there was an increase in sphingolipids such as ceramides and other metabolites such as iron. Compared to other cells, neurons consume a lot of cellular energy and so, these alterations are expected to impair neuronal function in mecr mutants and MEPAN patients.”
Dr. Debdeep Dutta, Postdoctoral Associate, Texas Children’s Hospital
Bellen added, “We were most intrigued to see increased levels of ceramide and defects in iron metabolism in fly models of MEPAN syndrome and in cells derived from these patients. Several previous studies from our lab and others had reported comparable increases in these metabolites in patients and fly models of other progressive neurodegenerative disorders such as Fredreich’s Ataxia, Infantile Neuroaxonal Dystrophy, Gaucher’s disease, and Parkinson’s disease.”
“Yet again, this work underscores the critical importance of maintaining the correct levels of mitochondrial fatty acids, ceramides, and iron to prevent a premature loss of neurons. We are hopeful findings from this study will advance drug development efforts for patients with MEPAN syndrome and related neurodegenerative disorders,” he concluded.
Source:
Journal reference:
Dutta, D., et.al. (2023). A defect in mitochondrial fatty acid synthesis impairs iron metabolism and causes elevated ceramide levels. Nature Metabolism. doi.org/10.1038/s42255-023-00873-0