Reviewed by Danielle Ellis, B.Sc.Nov 7 2023
Chronic rhinosinusitis (CRS) is an inflammatory condition affecting the nasal cavity and sinuses, which can be categorized into eosinophilic and non-eosinophilic subtypes.
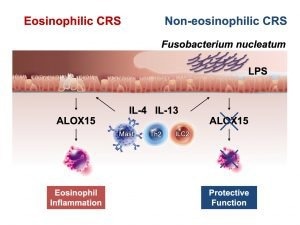 Experiments conducted in a recent study by researchers from Japan suggest that the lipopolysaccharides (LPS) produced by the bacterial species F. nucleatum suppresses the expression of ALOX15 and prevents excessive infiltration of eosinophils, which causes eosinophilic CRS, into nasal cells. Image Credit: University of Fukui.
Experiments conducted in a recent study by researchers from Japan suggest that the lipopolysaccharides (LPS) produced by the bacterial species F. nucleatum suppresses the expression of ALOX15 and prevents excessive infiltration of eosinophils, which causes eosinophilic CRS, into nasal cells. Image Credit: University of Fukui.
However, the knowledge of the nasal microbiome's involvement in the development of these conditions remains limited. In a recent investigation, Japanese researchers have unveiled a potential protective role of the bacterium Fusobacterium nucleatum in patients with non-eosinophilic CRS, shedding light on the mechanisms behind allergic diseases.
Japan, like many other countries worldwide, has experienced a concerning rise in the prevalence of chronic rhinosinusitis (CRS) over the past decade.
CRS, characterized by persistent inflammation lasting at least 12 weeks, can lead to symptoms such as nasal congestion, discharge, impaired nasal breathing, facial pain, and even loss of the sense of smell. Regrettably, addressing CRS is challenging due to its diverse manifestations.

Image Credit: BlurryMe/Shutterstock.com
CRS can be divided into two main categories: eosinophilic CRS (ECRS) and non-eosinophilic CRS (non-ECRS). ECRS is characterized by an elevated presence of eosinophils, a type of white blood cell that releases inflammatory compounds, in the nasal and sinus tissues.
The rising prevalence of CRS is primarily attributed to environmental factors influenced by changes in lifestyle. Among these environmental factors, the impact of microorganisms residing in the nasal cavity and passages on human health is well-recognized. However, it remains uncertain whether the nasal microbiome plays a role in the development of ECRS.
To address this knowledge gap, a research team led by Assistant Professor Masanori Kidoguchi from the Faculty of Medical Science at the University of Fukui, Japan, recently conducted a study on CRS within the Japanese population, with a specific focus on the nasal microbiome.
Their study, co-authored by Professor Shigeharu Fujieda from the University of Fukui and Professor Emiko Noguchi from the University of Tsukuba, was reported in The Journal of Allergy and Clinical Immunology on September 25th, 2023.
We undertook this study because the pathological functions of bacteria and their metabolites in the development of ECRS remain unknown.”
Masanori Kidoguchi, Assistant Professor, Faculty of Medical Science, University of Fukui
To begin their study, the researchers obtained nasal swabs from a total of 143 subjects, comprising 65 individuals with ECRS, 45 with non-ECRS, and 33 healthy control subjects.
Subsequently, they conducted a comparative analysis of microbiome diversity between the CRS and control groups using these samples, uncovering noteworthy distinctions that strongly indicate the involvement or influence of the nasal microbiome in the disease.
More significantly, the composition of the microbiome exhibited considerable differences between the ECRS and non-ECRS groups. Employing chemical and genetic testing, the research team identified a diminished presence of the bacterium Fusobacterium nucleatum (F. nucleatum) in ECRS patients.
Additionally, metagenomic assessments revealed a greater synthesis of lipopolysaccharide (LPS) in non-ECRS patients compared to those with ECRS.
F. nucleatum is known to cause inflammation by producing LPS. Some studies suggest that LPS has varying structures and functions depending on the bacterial species. We therefore hypothesized that LPS derived from F. nucleatum might be linked to the pathogenesis of both ECRS and non-ECRS.”
Masanori Kidoguchi, Assistant Professor, Faculty of Medical Science, University of Fukui
To evaluate this hypothesis, the research team conducted investigations to determine whether lipopolysaccharide (LPS) extracted from Fusobacterium nucleatum had any impact on the expression of specific cytokines within human bronchial epithelial cell cultures.
Their experiments demonstrated that F. nucleatum-specific LPS effectively suppressed the expression of ALOX15, an enzyme crucial in the development of nasal polyps and eosinophil-related inflammation.
In summary, the findings from this study suggest that disturbances in the nasal microbiome likely play a pivotal role in eosinophilic chronic rhinosinusitis (ECRS). This discovery holds the potential for developing more effective strategies to address this challenging condition.
The microbiome may strongly influence treatment resistance in CRS and may have an impact on other allergic diseases as well. Future studies will hopefully lead to probiotic development and lifestyle modification methods for preventing refractory chronic sinusitis.”
Masanori Kidoguchi, Assistant Professor, Faculty of Medical Science, University of Fukui
One can anticipate that gaining a deeper comprehension of these inflammatory conditions will lead to the development of treatments and prevention approaches aimed at enhancing the quality of life for individuals suffering from ECRS.
Source:
Journal reference:
Kidoguchi, M., et al. (2023) Middle meatus microbiome in patients with eosinophilic chronic rhinosinusitis in a Japanese population. Journal of Allergy and Clinical Immunology. doi.org/10.1016/j.jaci.2023.06.029