Scientists at McMaster University have identified distinct features of a mechanism employed by bacteria to withstand a crucial category of antibiotics.
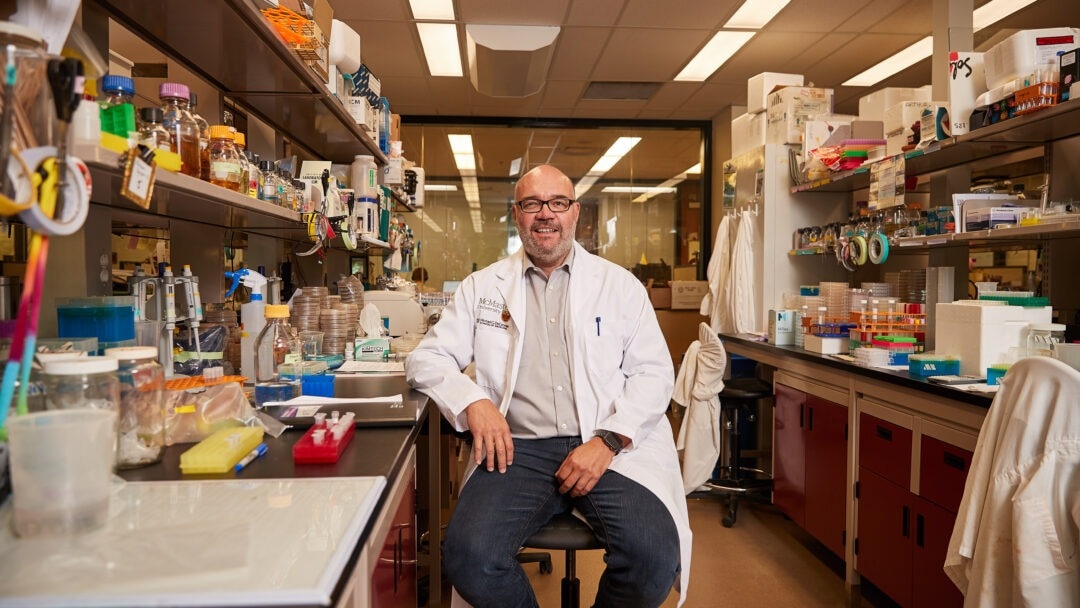 Gerry Wright, professor of Biochemistry and Biomedical studies at McMaster, says his lab’s recent discovery is significant because the antibiotic apramycin is currently in clinical trials and, should it pass through, having a thorough understanding of how bacteria might resist the drug will be crucial to extending its utility. Image Credit: Blake Dillon.
Gerry Wright, professor of Biochemistry and Biomedical studies at McMaster, says his lab’s recent discovery is significant because the antibiotic apramycin is currently in clinical trials and, should it pass through, having a thorough understanding of how bacteria might resist the drug will be crucial to extending its utility. Image Credit: Blake Dillon.
The recent publication in the esteemed journal Nature Chemical Biology highlights groundbreaking research revealing that resistance to aminoglycoside drugs, commonly used to treat various infections, is significantly more intricate than previously believed.
Gerry Wright, the Lead Investigator and Professor of Biochemistry and Biomedical Sciences at McMaster reports that his team observed unprecedented versatility in the ApmA gene, a well-studied bacterial resistance gene.
The study demonstrates that this gene, atypically, empowers bacteria to execute different functions against various antibiotics. Among the numerous aminoglycoside resistance enzymes identified by researchers, Wright emphasizes that only this particular one has displayed such adaptable behavior.
It’s a unicorn. It looks different, it operates differently, and it belongs to an entirely different family of enzymes. It’s completely different from all of the resistance mechanisms that we associate with this class of antibiotic.”
Gerry Wright, Study Lead Investigator and Professor, Biochemistry and Biomedical Sciences, McMaster University
As a member of the Michael G. DeGroote Institute for Infectious Disease Research, Wright notes that aminoglycosides were among the earliest clinically relevant antibiotics and the first effective ones against tuberculosis. However, due to their prescription since the 1940s, he highlights that “resistance to them has become a real issue”— with the exception of apramycin.
The antibiotic apramycin avoids most mechanisms of resistance, and so it is a strong candidate for new clinical applications. Unfortunately, this mechanism that we’ve been studying is not one that the drug can avoid.”
Gerry Wright, Study Lead Investigator and Professor, Biochemistry and Biomedical Sciences, McMaster University
According to Wright, the recent breakthrough in his lab is noteworthy because apramycin is presently undergoing clinical trials. If it successfully progresses through these trials, possessing a comprehensive understanding of how bacteria could develop resistance to the drug will be essential in maximizing its effectiveness.
If we’re going to bring this drug to market, then we better know what the enemy is. Learning more about this unique resistance mechanism could inform follow-on research into next-generation apramycin or diagnostics that could detect ApmA in bacteria.”
Gerry Wright, Study Lead Investigator and Professor, Biochemistry and Biomedical Sciences, McMaster University
Source:
Journal reference:
Bordeleau, E., et al. (2023) Mechanistic plasticity in ApmA enables aminoglycoside promiscuity for resistance. Nature Chemical Biology. doi.org/10.1038/s41589-023-01483-3.